Raja Lahiri provides an overview of coronary angiography. Key points include:
- Coronary angiography is the current gold standard for visualizing the coronary arteries through X-ray imaging with contrast injection.
- The history of coronary angiography began in the 1920s-1940s with early experiments in cerebral and cardiac catheterization.
- Modern techniques involve accessing arteries typically through the femoral or radial arteries to insert a catheter for contrast injection into the coronary arteries under X-ray imaging.
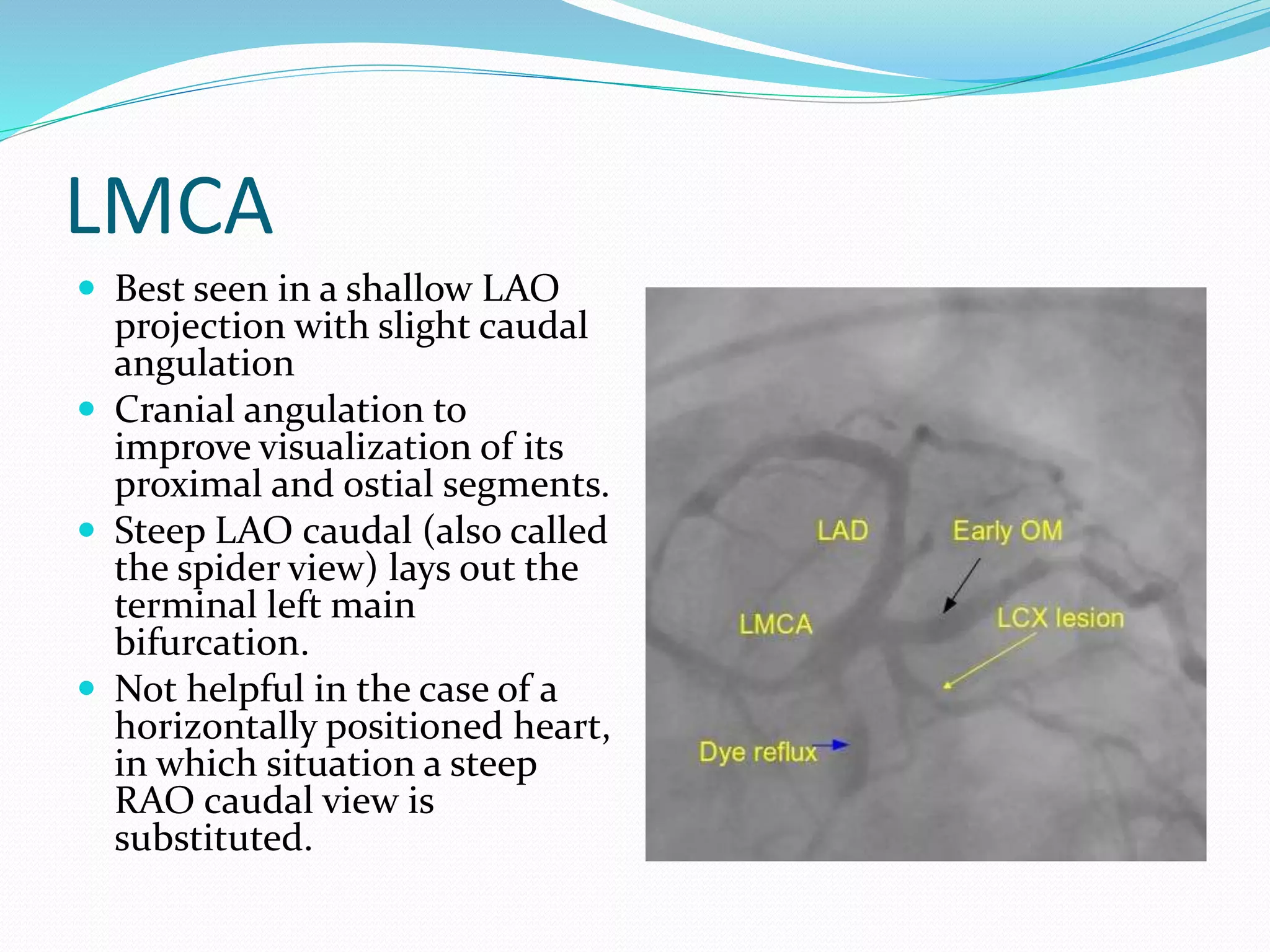
- Multiple angiographic views are needed to visualize different segments of the left and right coronary arteries. Coronary angiography is used to evaluate coronary artery disease, graft patency, and left ventricular function.