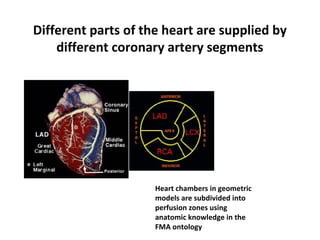
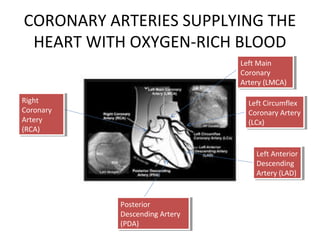
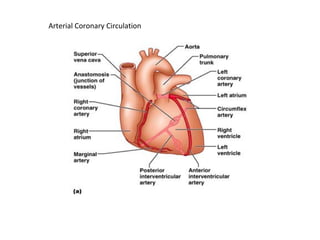
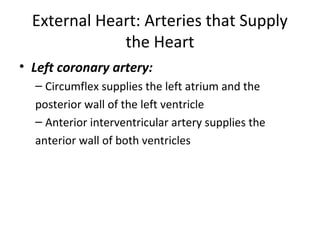
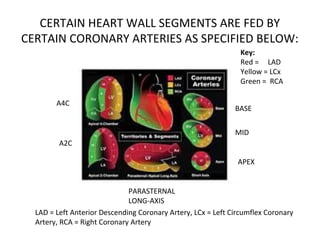
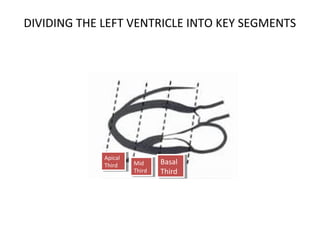
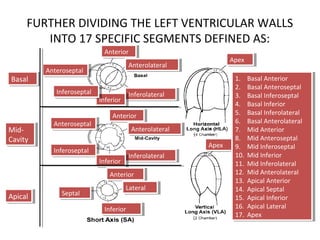
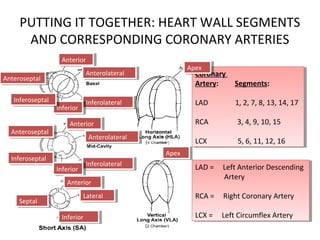
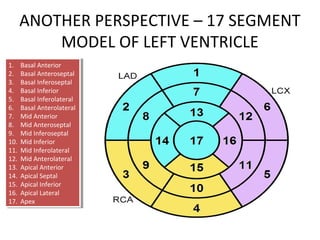
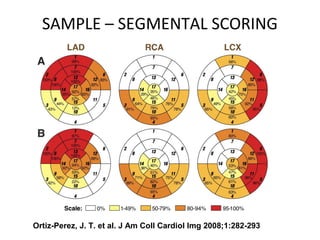
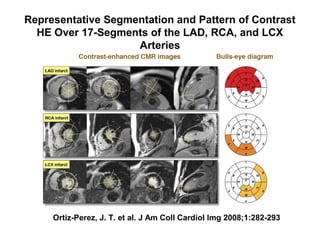
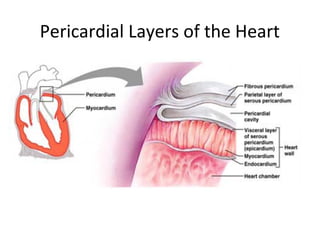
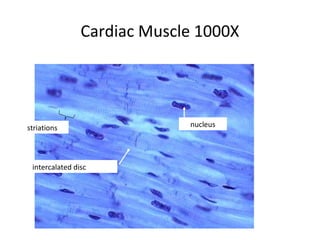
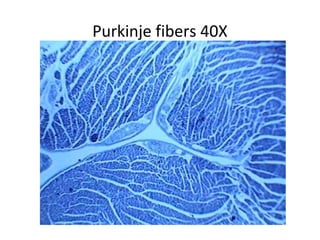
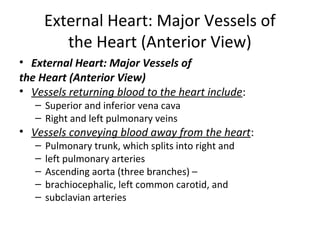
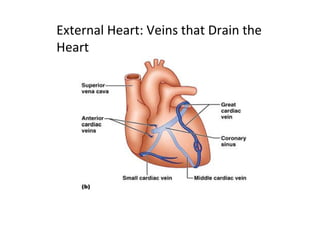
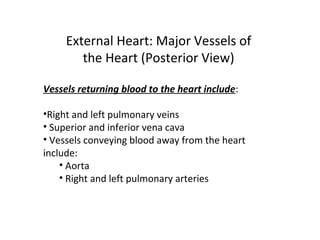
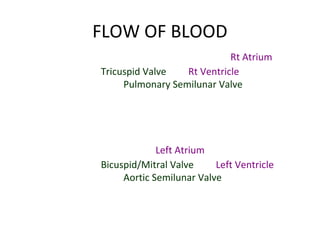
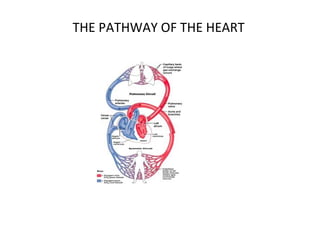
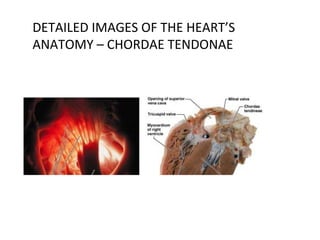
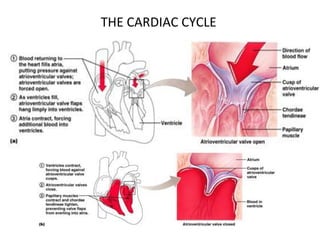
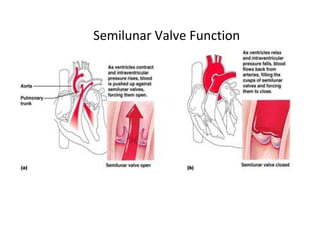
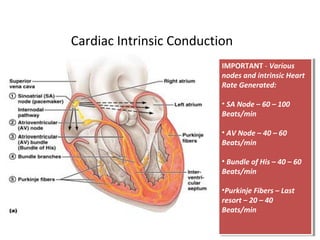
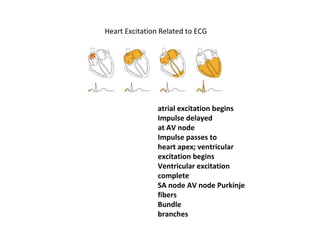
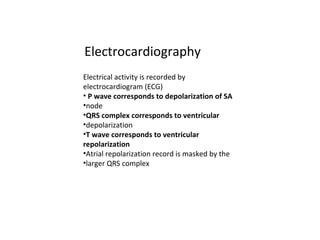
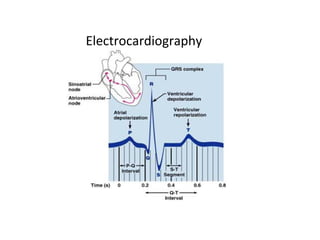
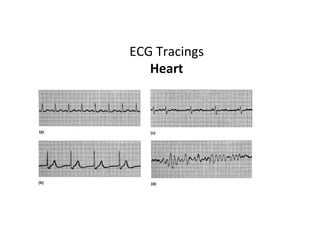
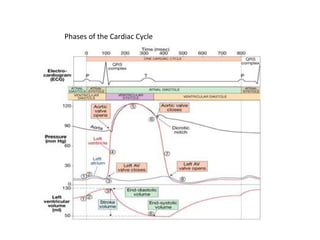
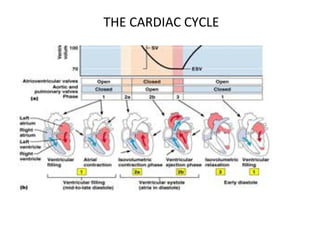
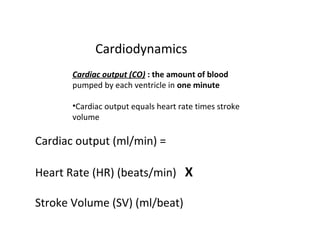
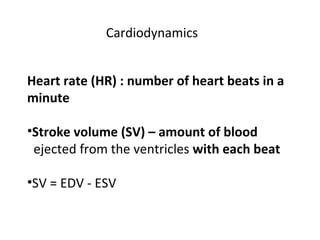
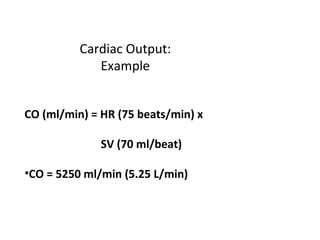
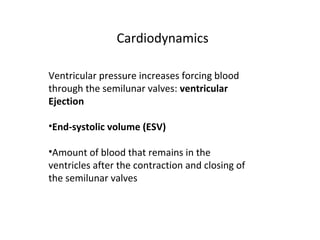
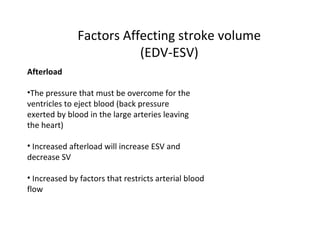
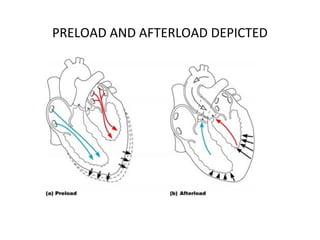
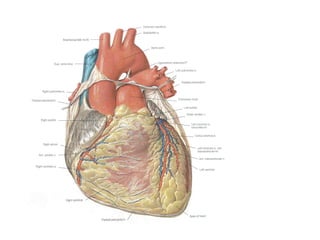
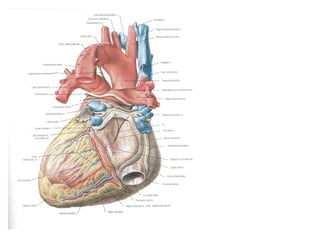
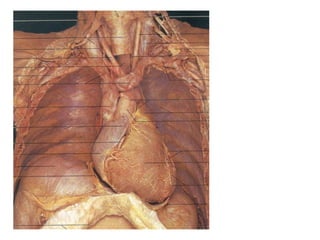
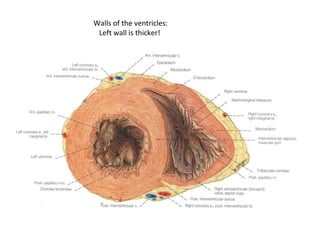
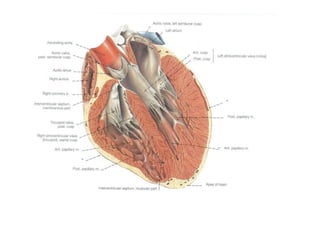
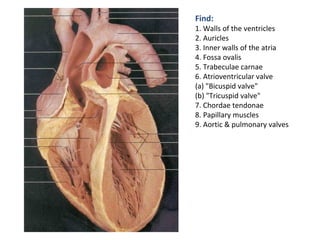
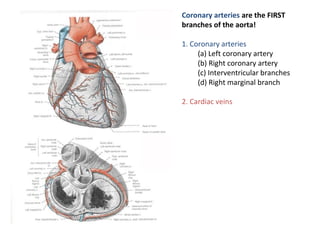
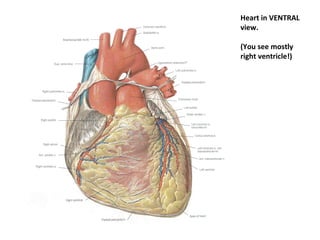
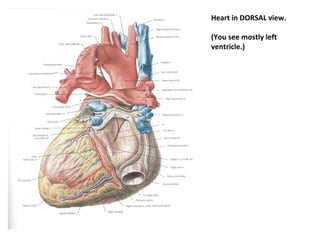
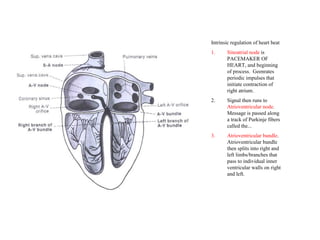
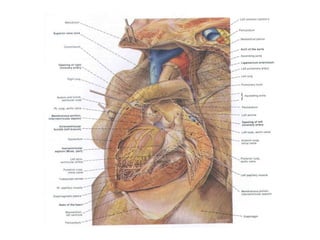
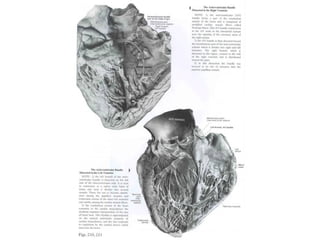
The document provides an extensive overview of the cardiovascular system, focusing on the anatomy and physiology of the heart, including its major arteries and veins, the pathway of blood flow, and the cardiac cycle. It details the functions of various coronary arteries and how different segments of the heart are supplied with blood, as well as the intrinsic conduction system regulating heartbeats. Additionally, it discusses factors affecting cardiac output and stroke volume alongside the structure of the heart and its coverings.