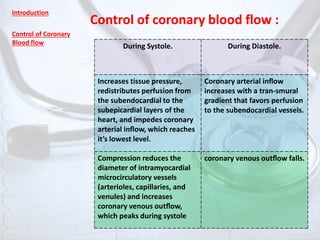
This document discusses coronary blood flow and its control. It begins by introducing the unique nature of the coronary circulation and the importance of balancing oxygen supply and demand. It then covers several topics in depth: the control of coronary blood flow during different parts of the cardiac cycle; the determinants of myocardial oxygen consumption; coronary autoregulation and how it can become impaired; transmural variations in coronary blood flow; endothelium-dependent modulation of coronary tone through factors like nitric oxide, prostacyclin, and endothelin; and the components of coronary vascular resistance. The overall goal is to provide an in-depth overview of coronary circulation and the factors that influence blood flow to the heart.