This document provides information about a seminar on hemodynamic monitoring presented by UMAdevi.k. It discusses the purpose of hemodynamic monitoring in critically ill patients, which is to continuously assess the cardiovascular system and diagnose/manage complex medical conditions. Specific techniques covered include arterial blood pressure monitoring, central venous pressure monitoring, and pulmonary artery catheter pressure monitoring. Key aspects of each technique like indications, equipment, procedures, nursing responsibilities, and potential complications are defined. Normal hemodynamic values are also provided.

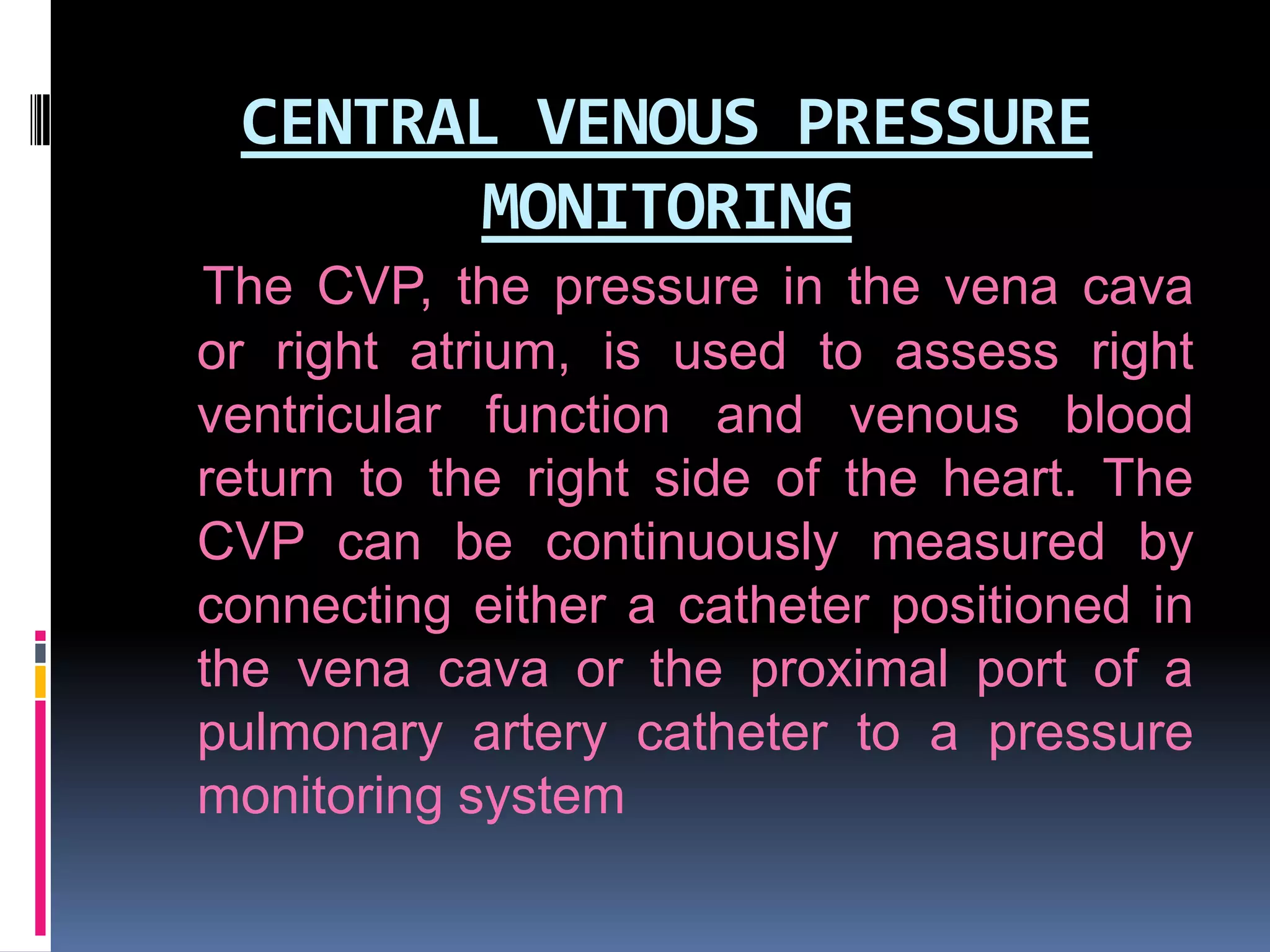
![DETERMINANTS OF CARDIAC
PERFORMNACE
PRELOAD (estimated by end diastolic
volume CVP for RVEDV ; PAOP (wedge)
pressure for LVEDV
AFTERLOAD (SVR = [MAP-CVP]/CO*80)
CONTRACTILITY](https://image.slidesharecdn.com/hemodynamicmonitoringppt-131023035424-phpapp02/75/Hemodynamic-monitoring-ppt-14-2048.jpg)


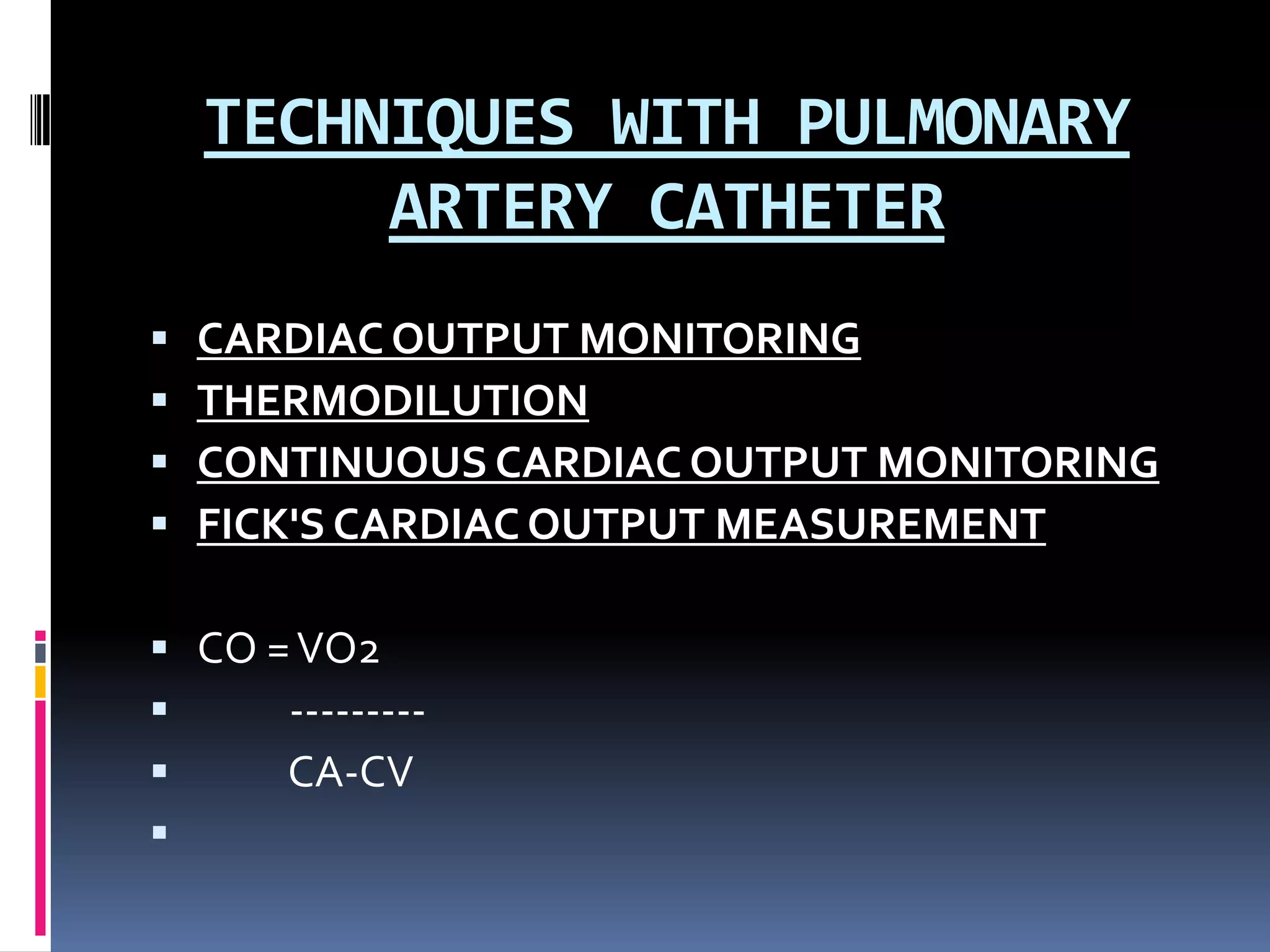
![DERIVED PARAMETERS
Cardiac o/p measurements may be combined with systemic
arterial, venous, and PAP determinations to calculate a number
of variables useful in assessing the overall hemodynamic status
of the patient.
They are,
Cardiac index = Cardiac output / Body surface area
Systemic vascular resistance = [(Mean arterial pressure -
resistance CVP or rt atrial pressure)/Cardiac output] x 80
Pulmonary vascular resistance = [(PAP - PAWP) / Cardiac
vascular resistance output] x 80
Mixed venous oxygen saturation (SvO2)
(SvO2 = SaO2 - [VO2 / (1.36 x Hb x CO)]
(6)](https://image.slidesharecdn.com/hemodynamicmonitoringppt-131023035424-phpapp02/75/Hemodynamic-monitoring-ppt-44-2048.jpg)