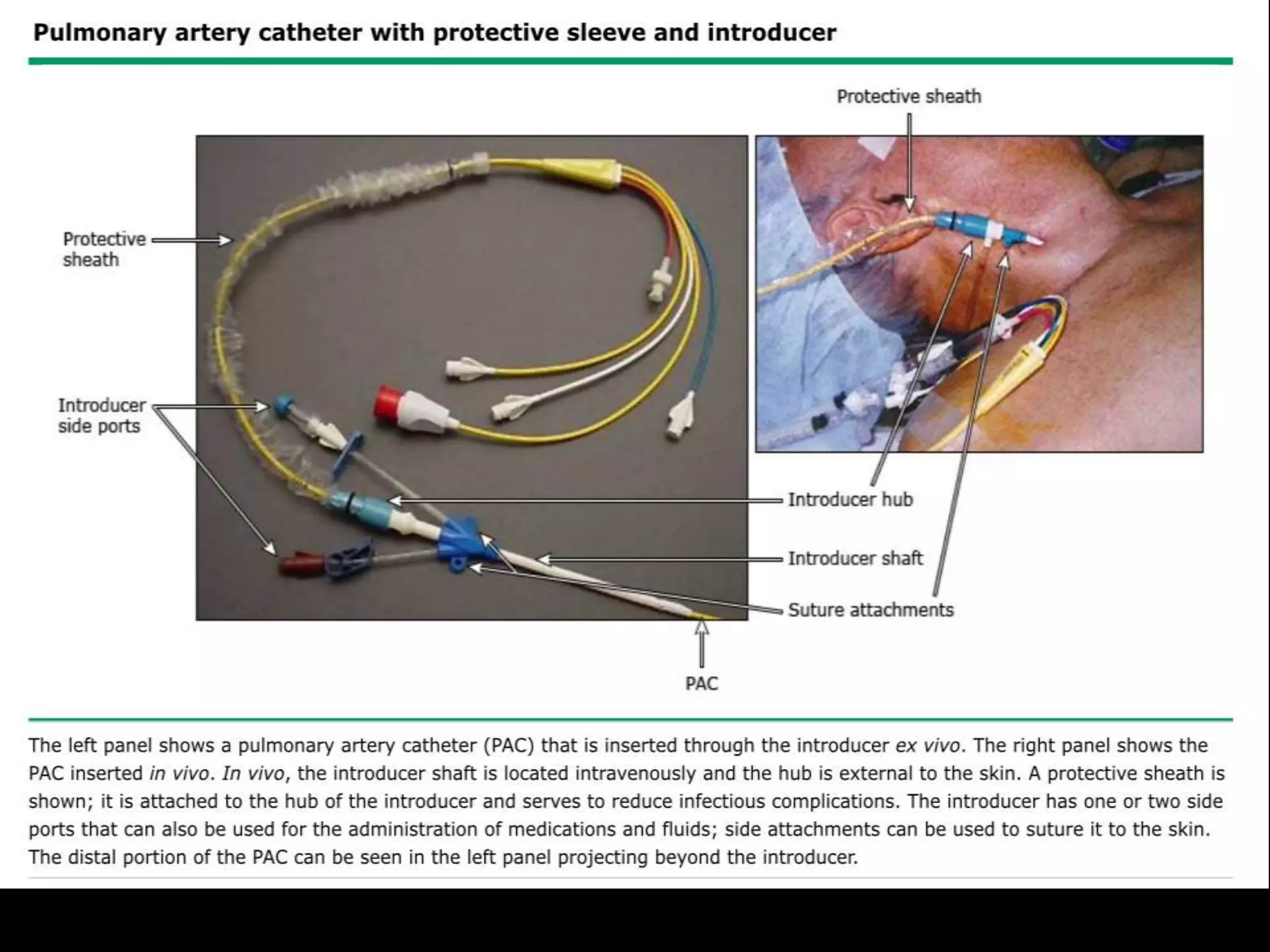
Pulmonary artery catheters (PAC), also known as Swan-Ganz catheters, are used to evaluate various medical conditions, especially in critical care settings despite declining routine use. They provide direct measurements such as cardiac output and pulmonary artery pressures, and are indicated for diagnostic and therapeutic purposes like managing shock and complications from surgery. The document outlines the technique, preparation, potential complications, and interpretation of hemodynamic values associated with PAC usage.