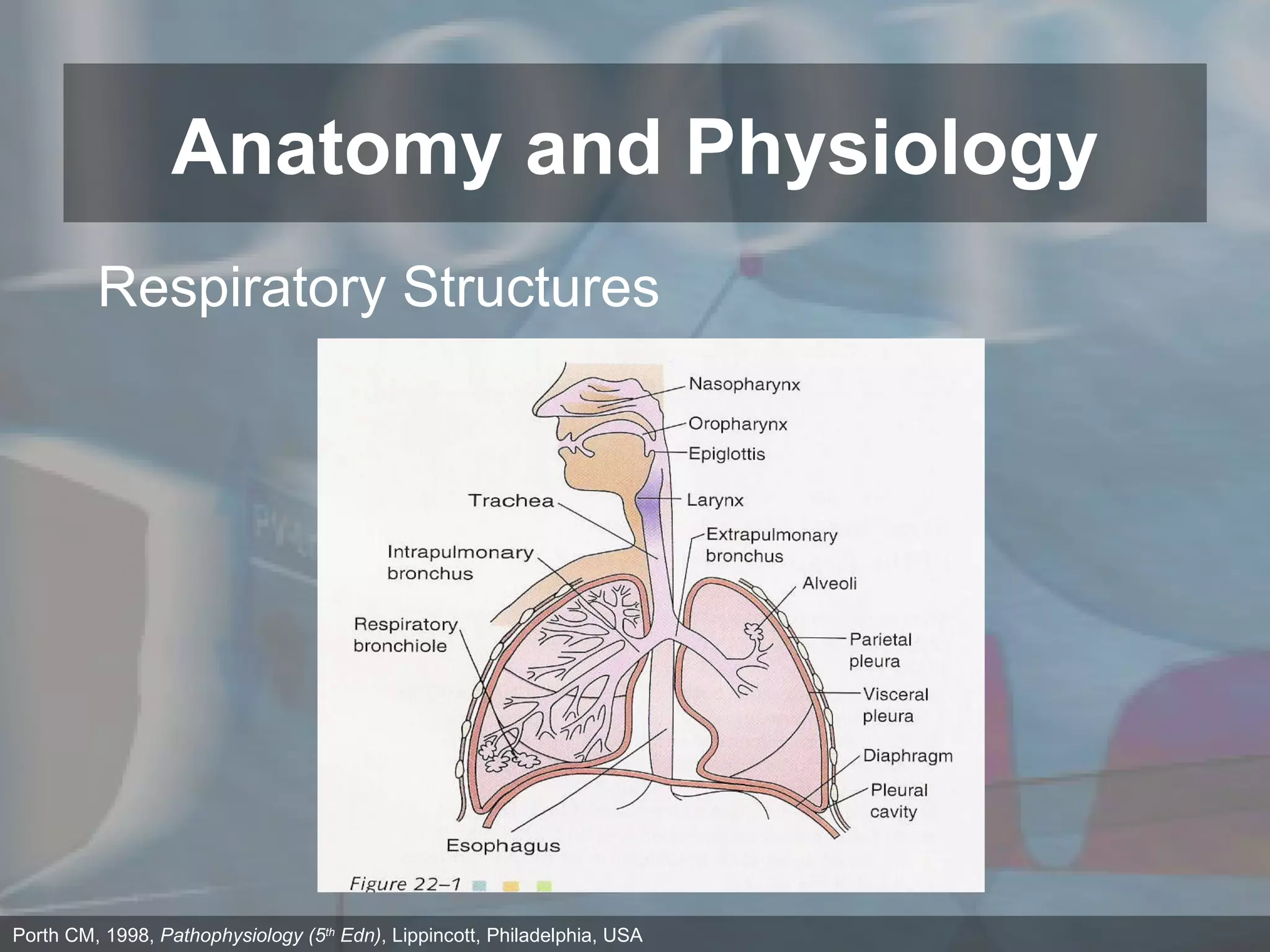
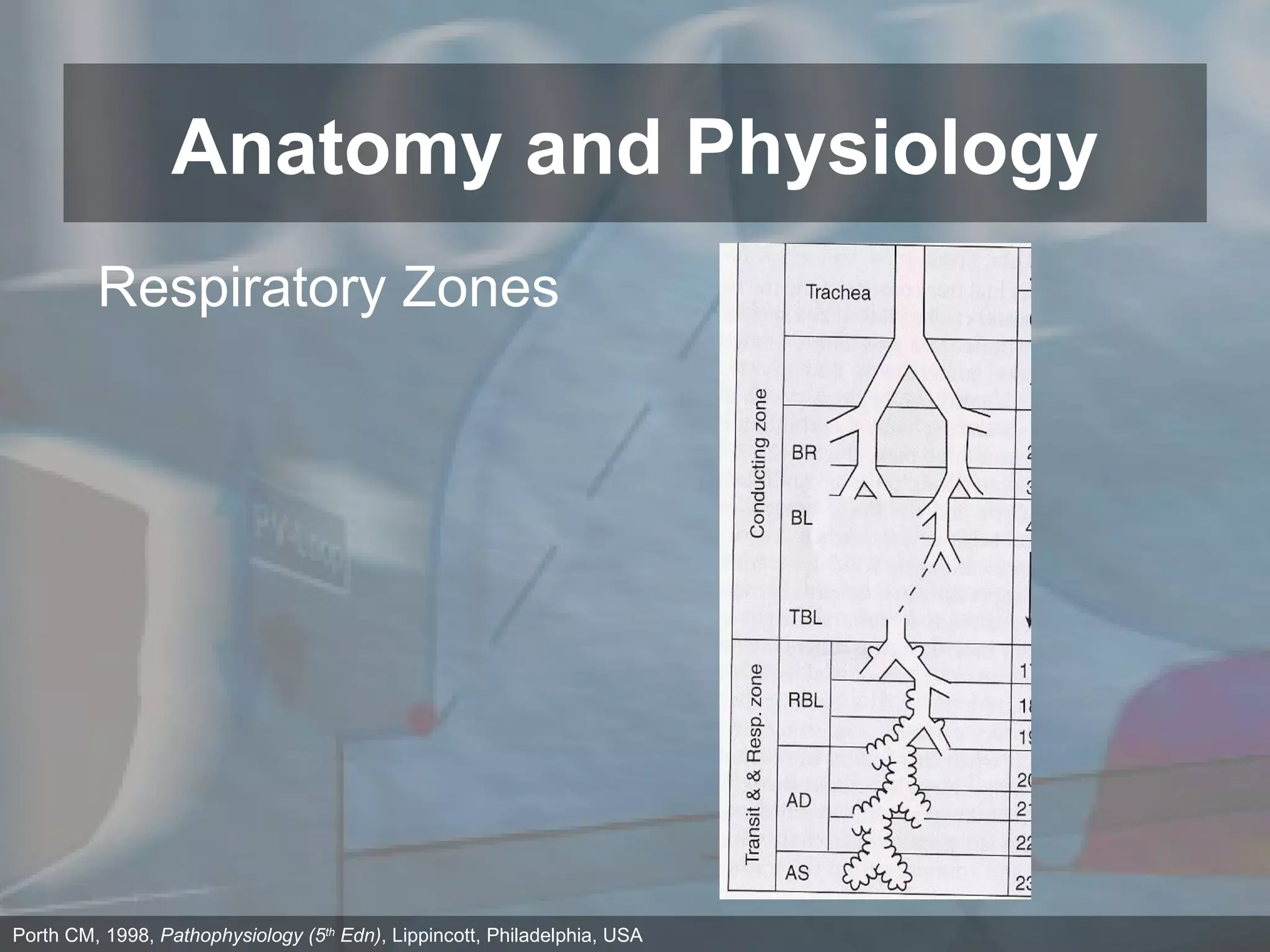
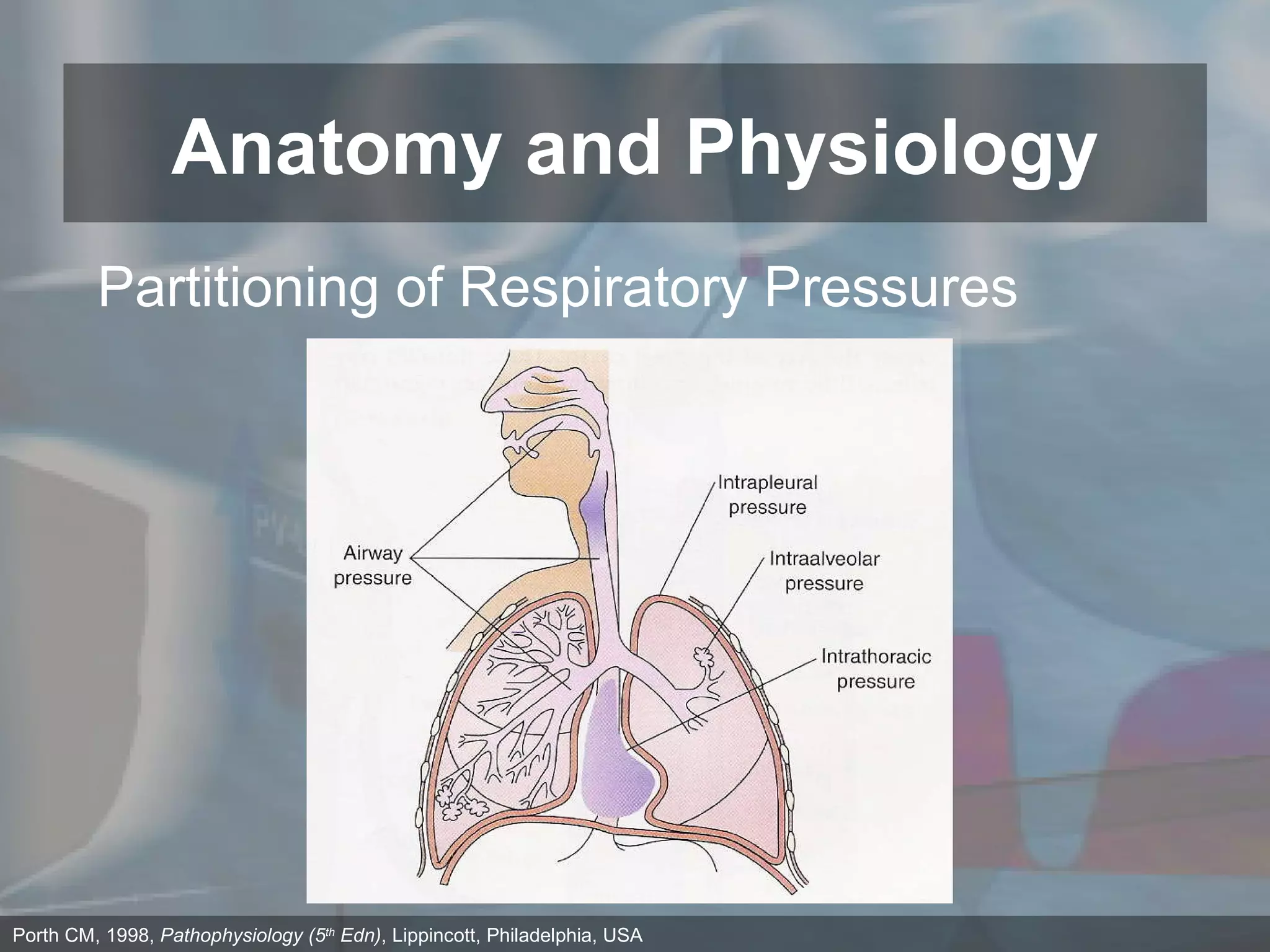
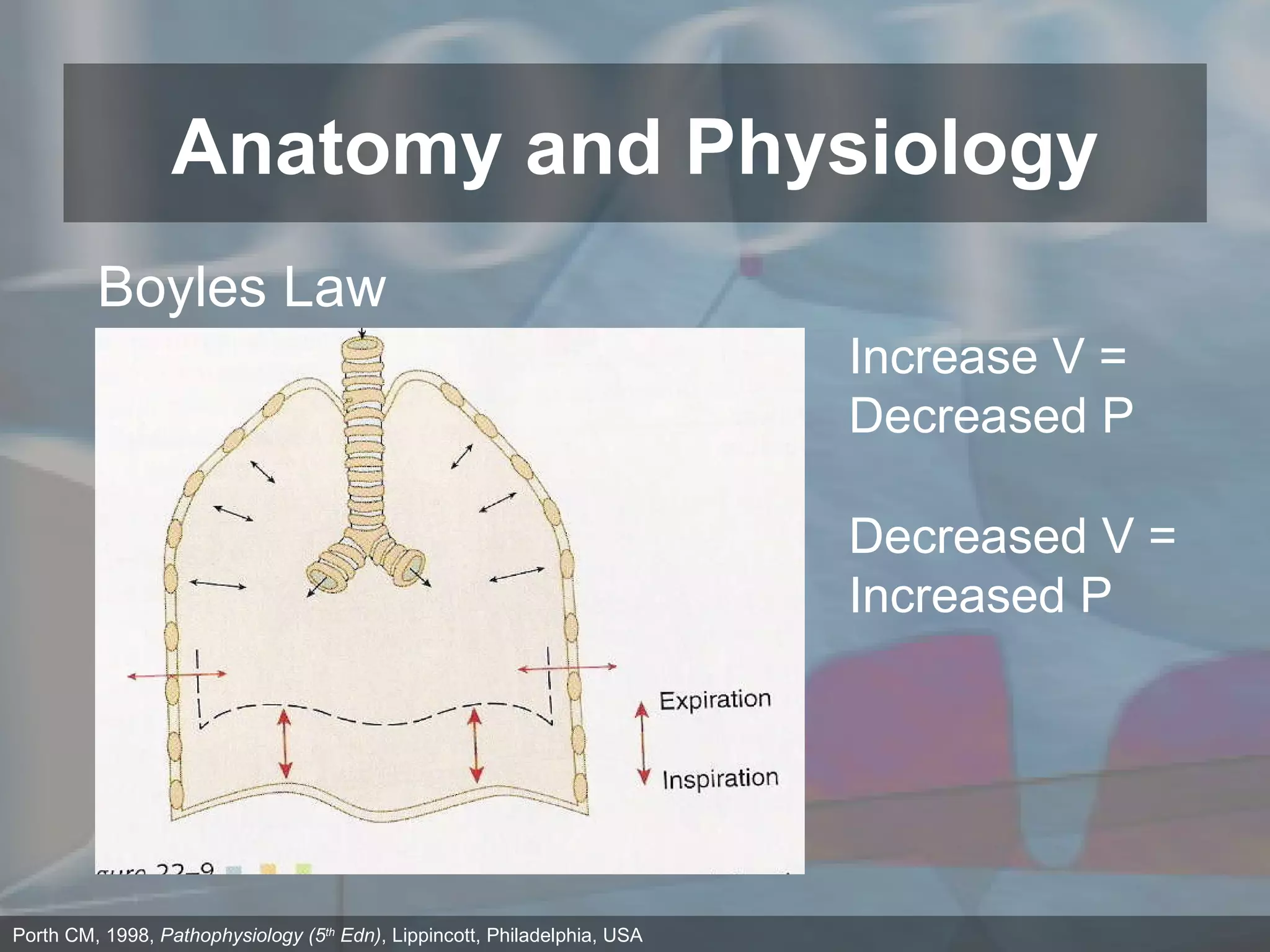
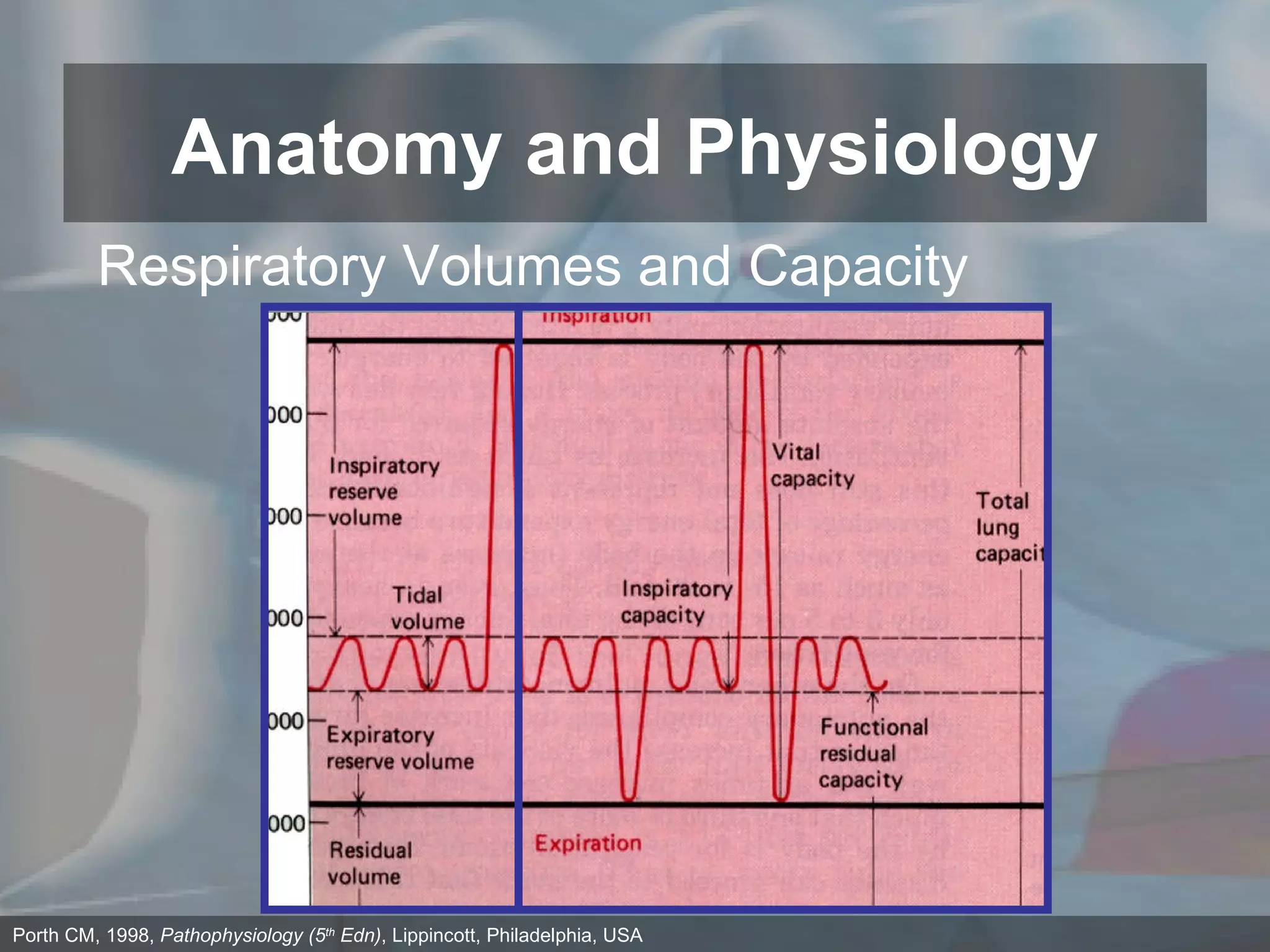
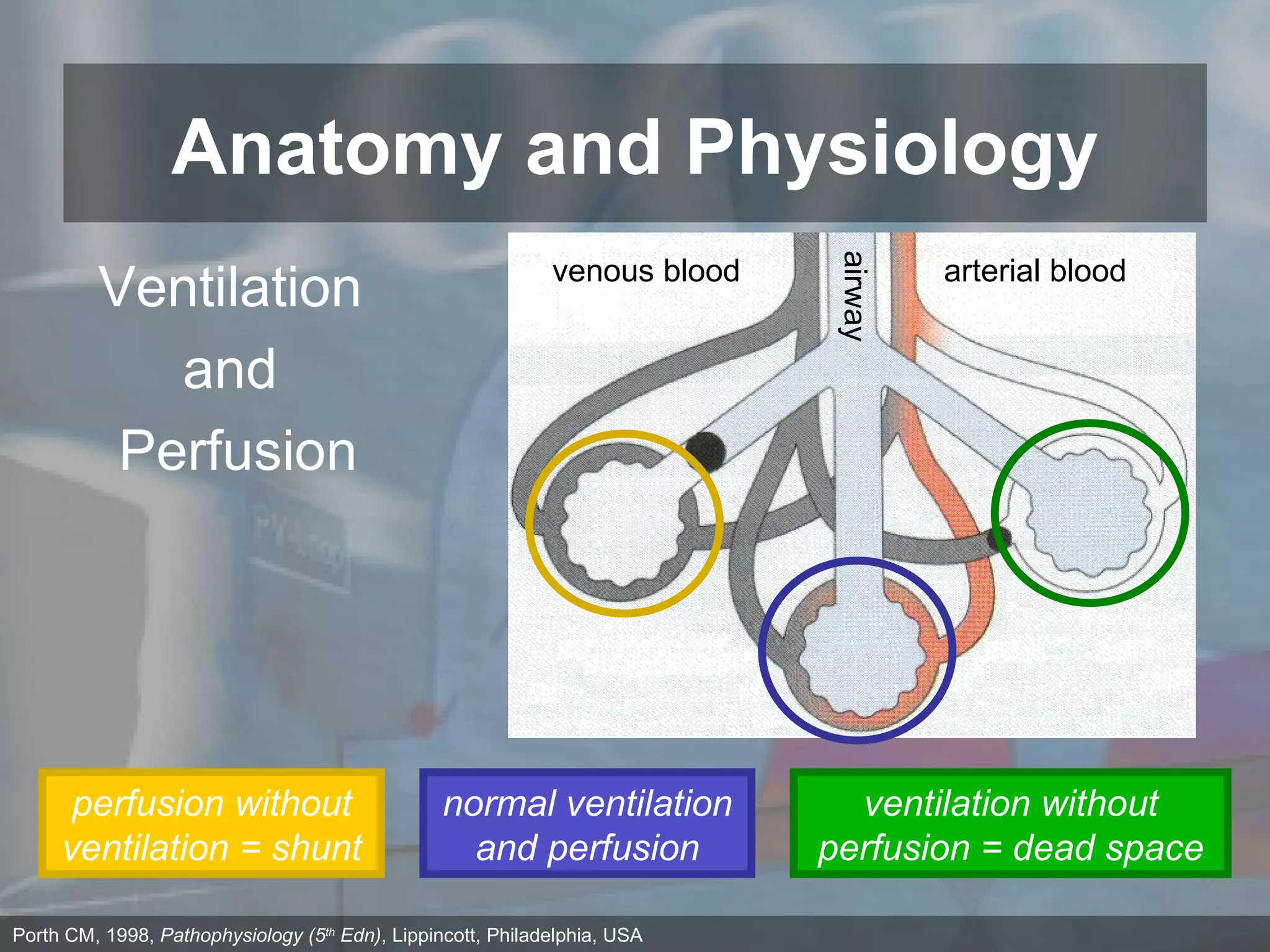
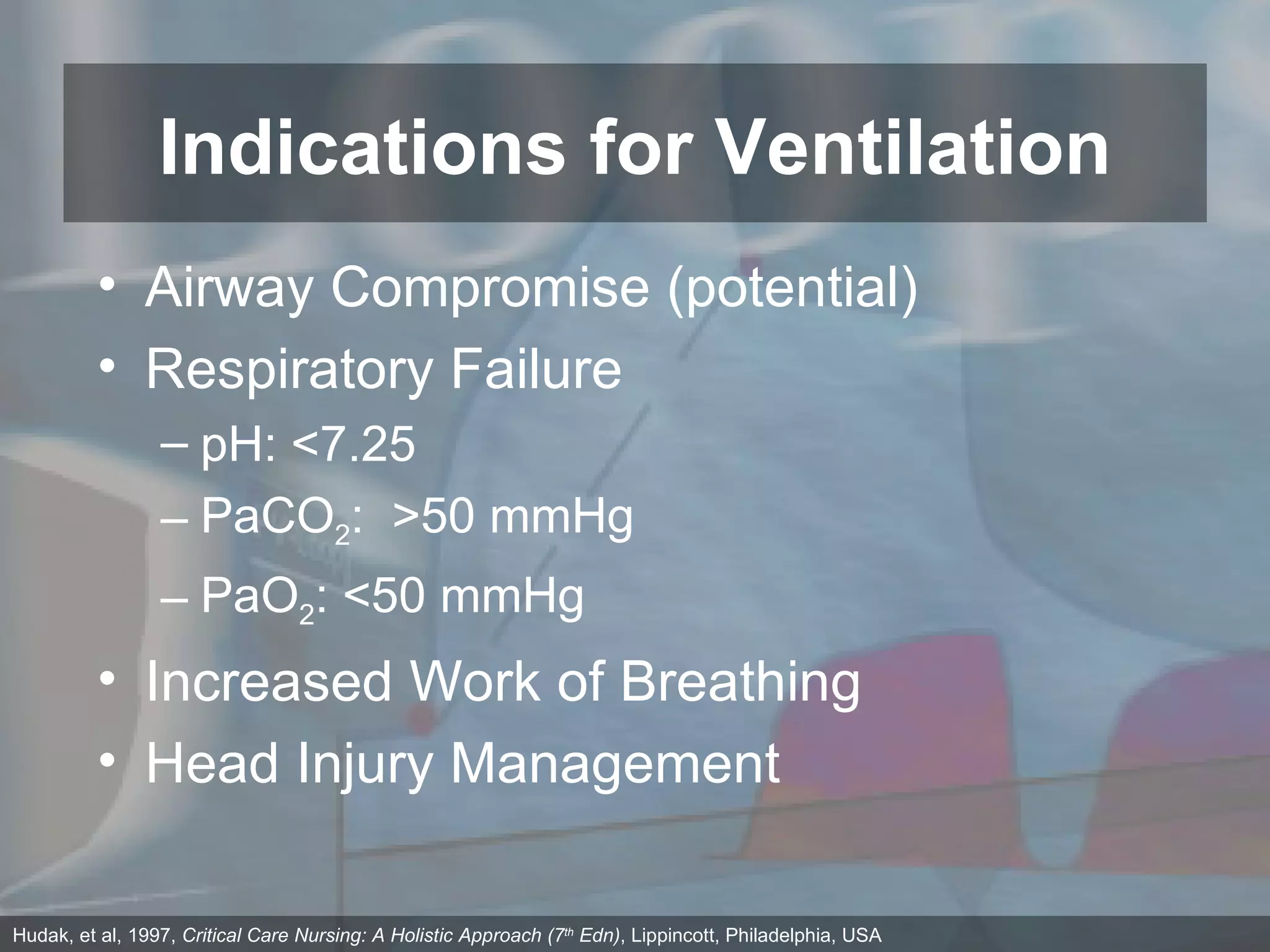
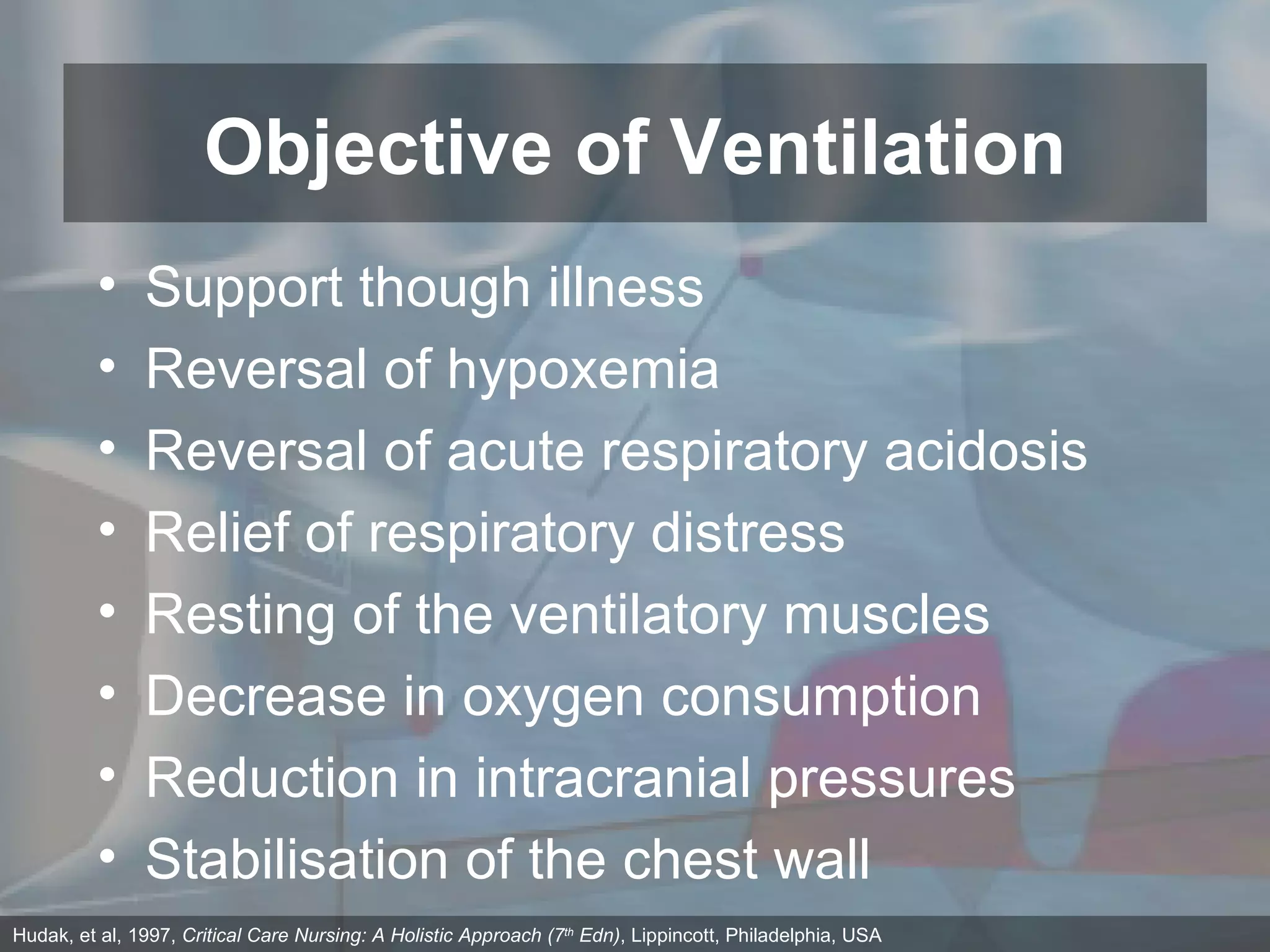
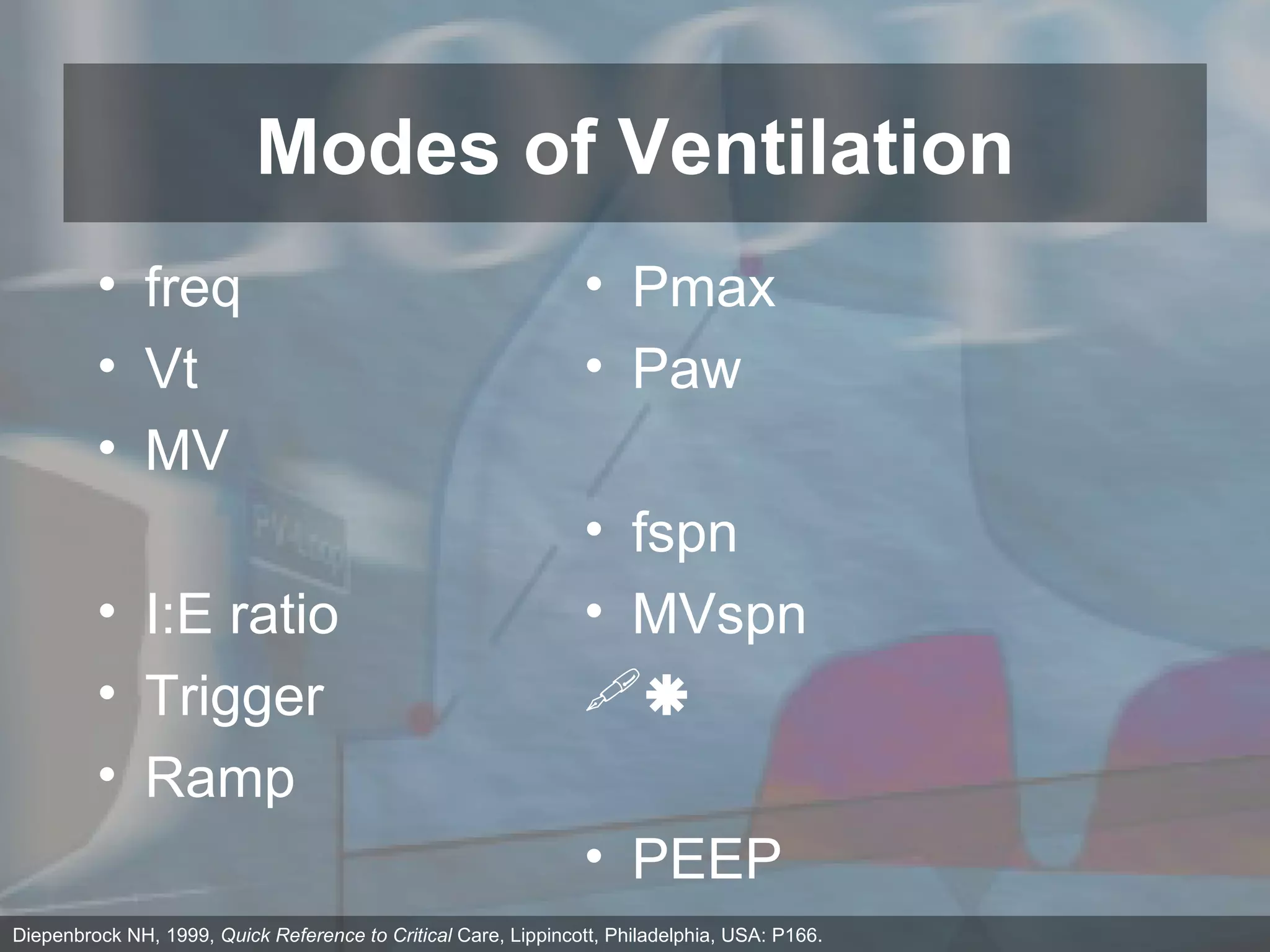
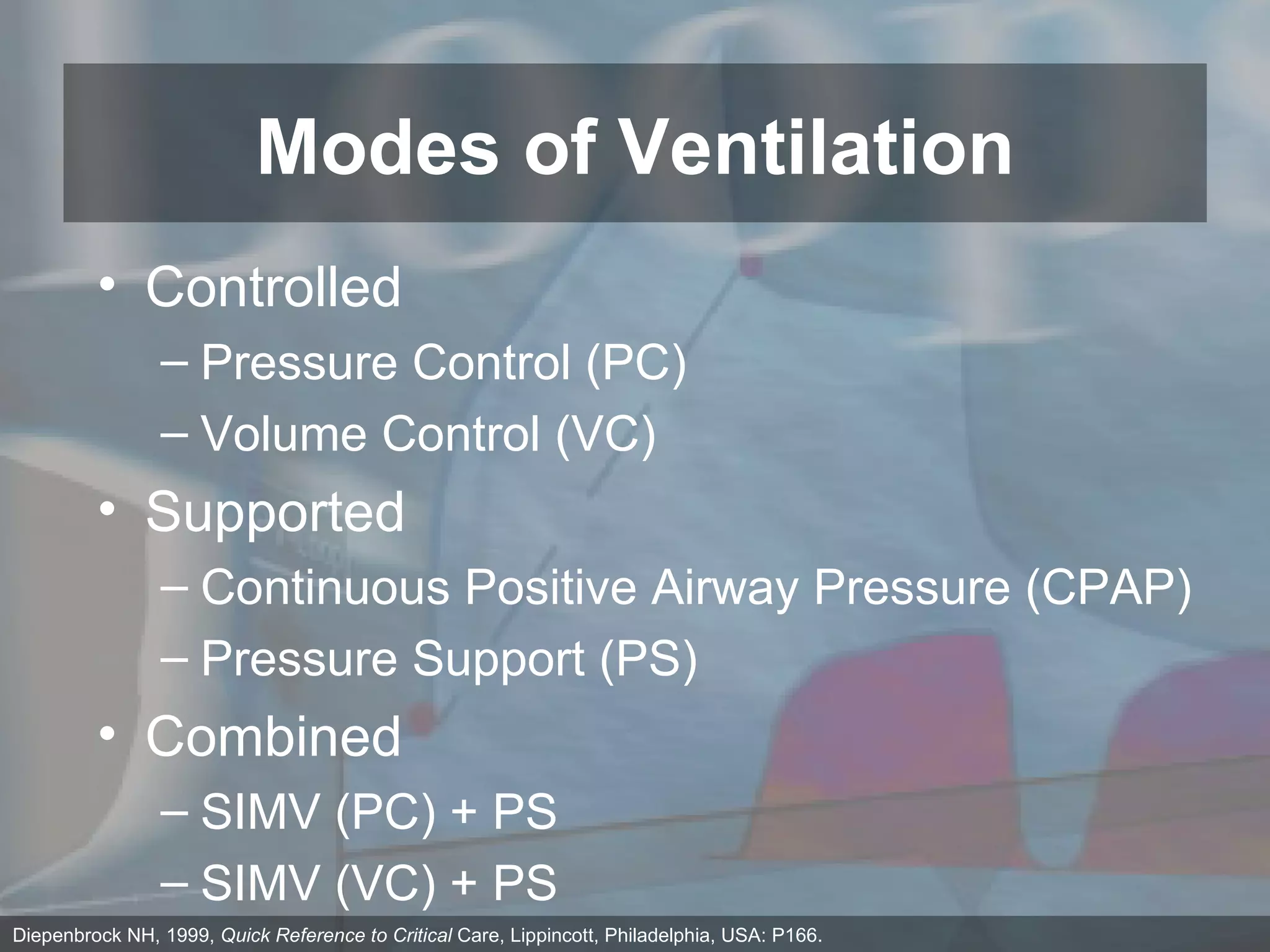
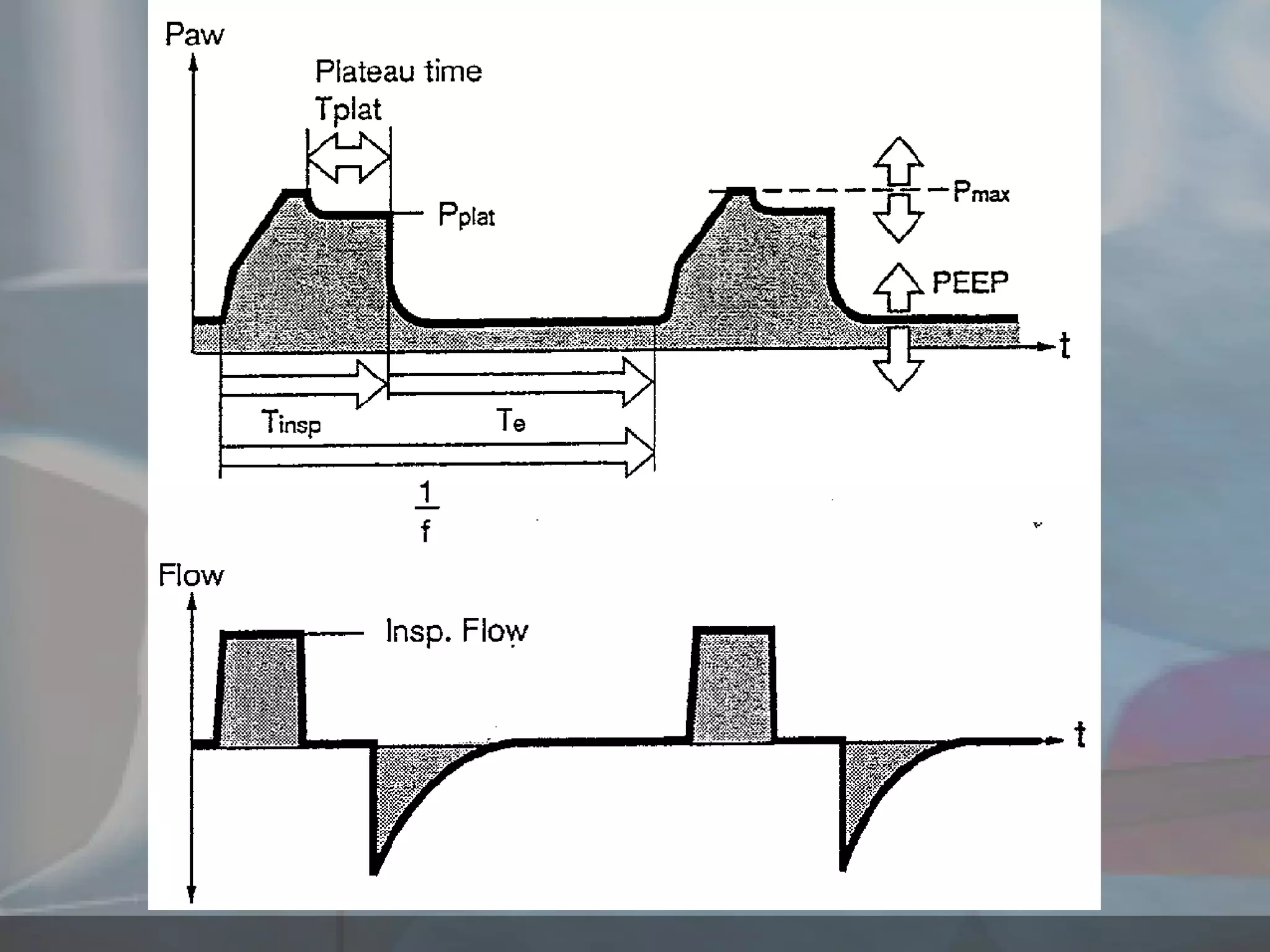
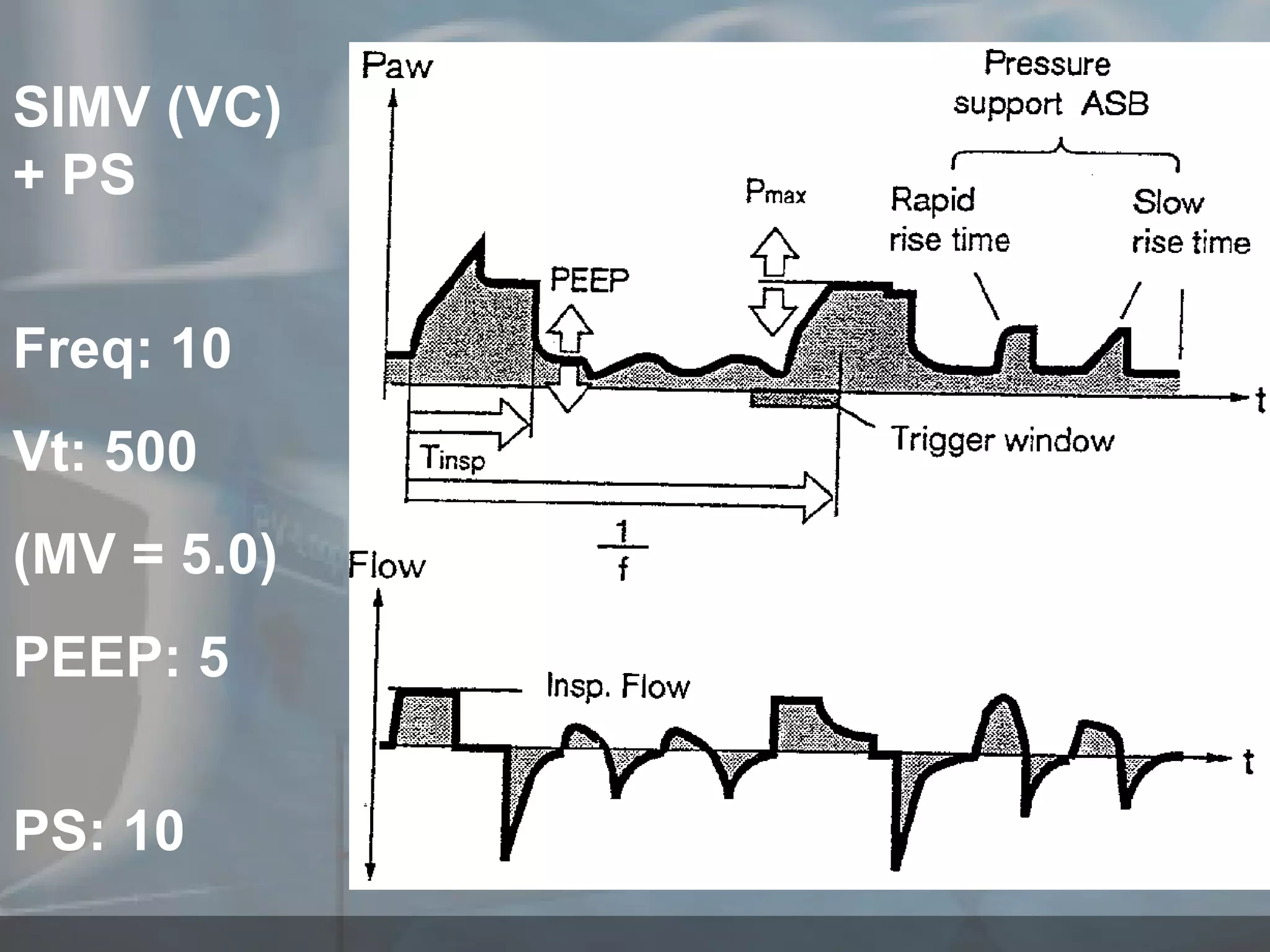
The document outlines the fundamental principles of ventilation, including respiratory anatomy and physiology, indications, modes of ventilation, and patient management. It discusses mechanics such as elasticity, compliance, and pressure, and explores various ventilation modes such as controlled mechanical ventilation and pressure support. Additionally, it addresses potential complications and the importance of monitoring and patient management strategies.