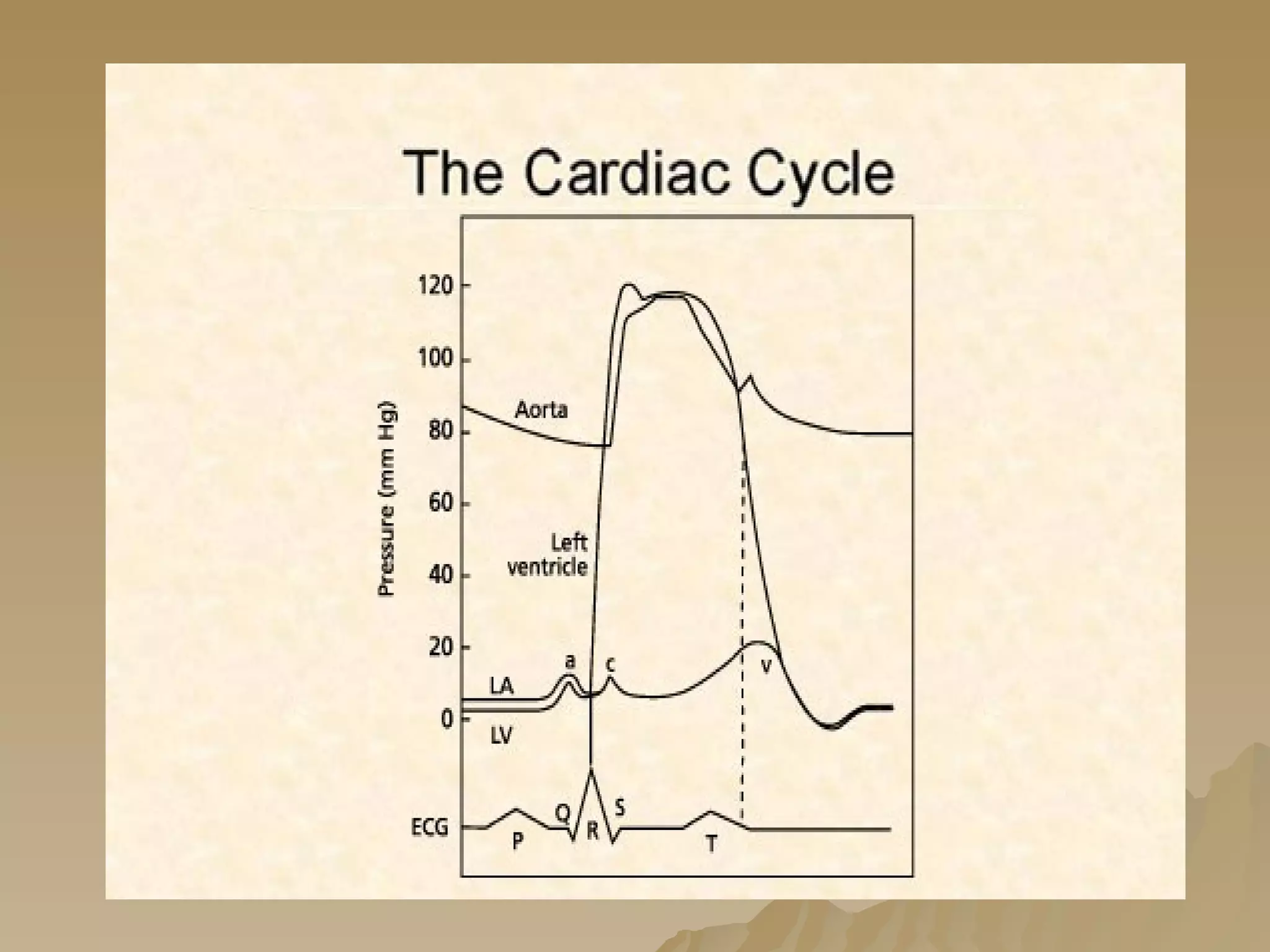
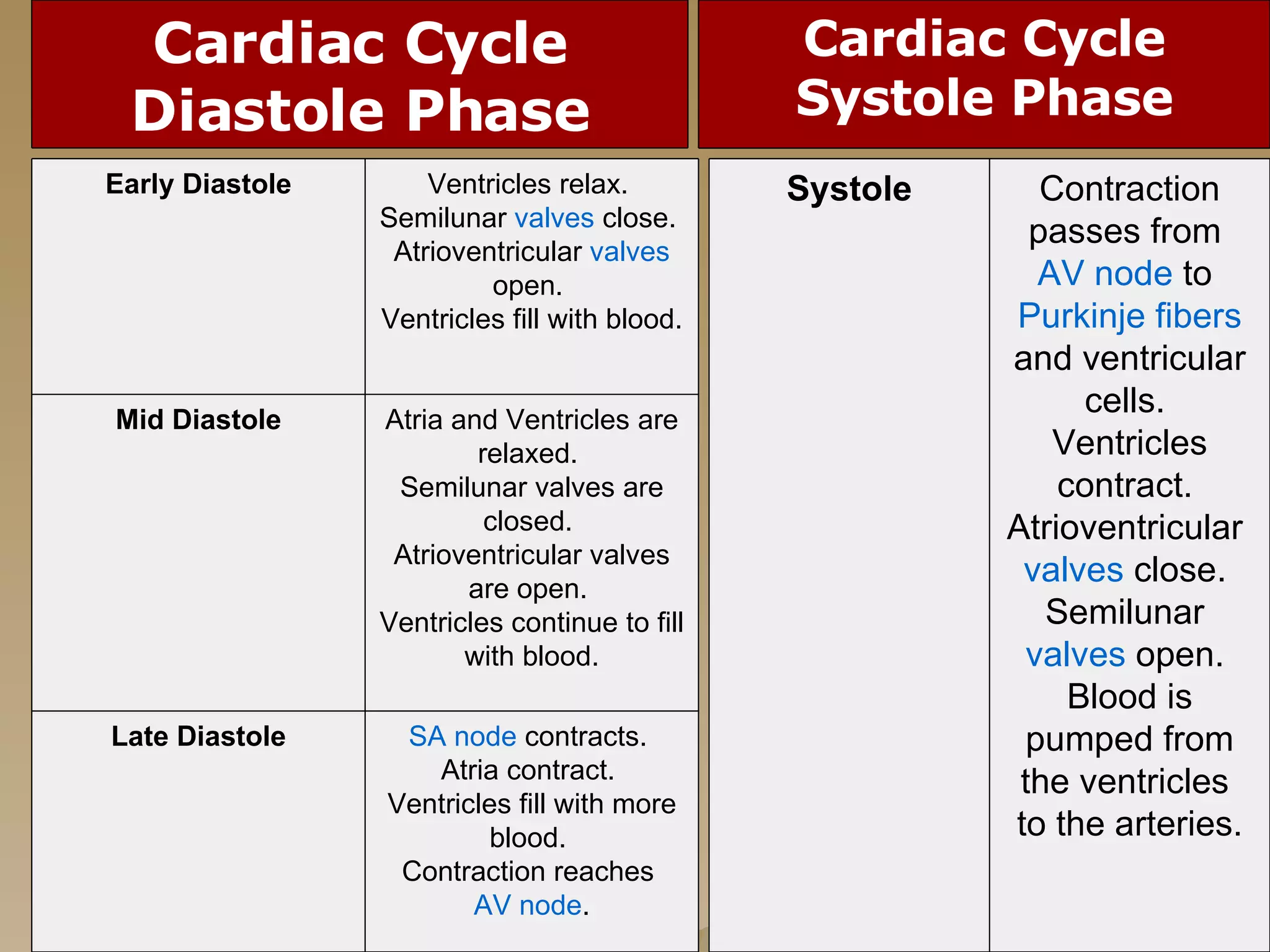
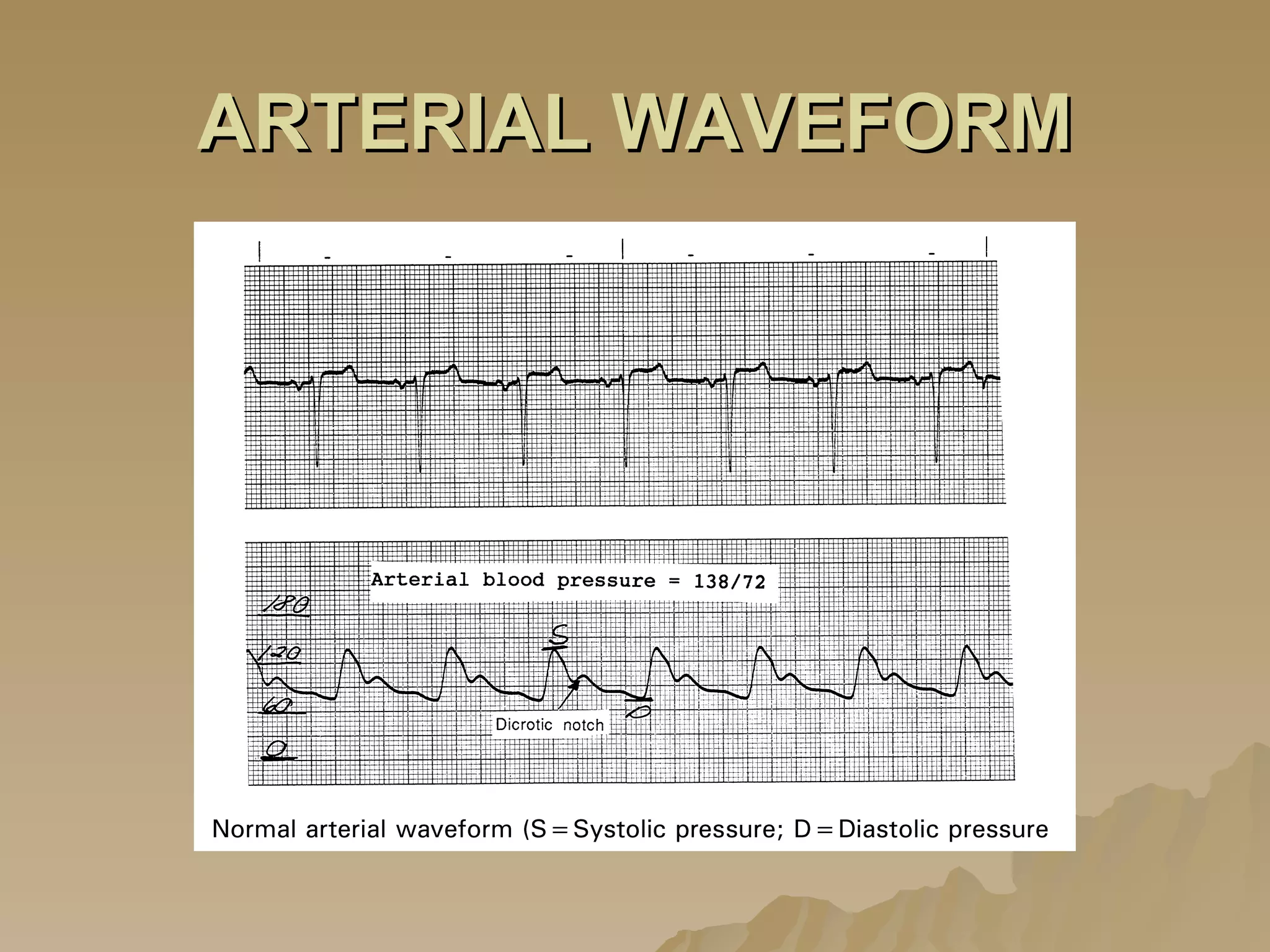
1. The purpose of invasive hemodynamic monitoring is to detect and treat life-threatening conditions such as heart failure and cardiac tamponade by evaluating a patient's cardiovascular function and response to treatment.
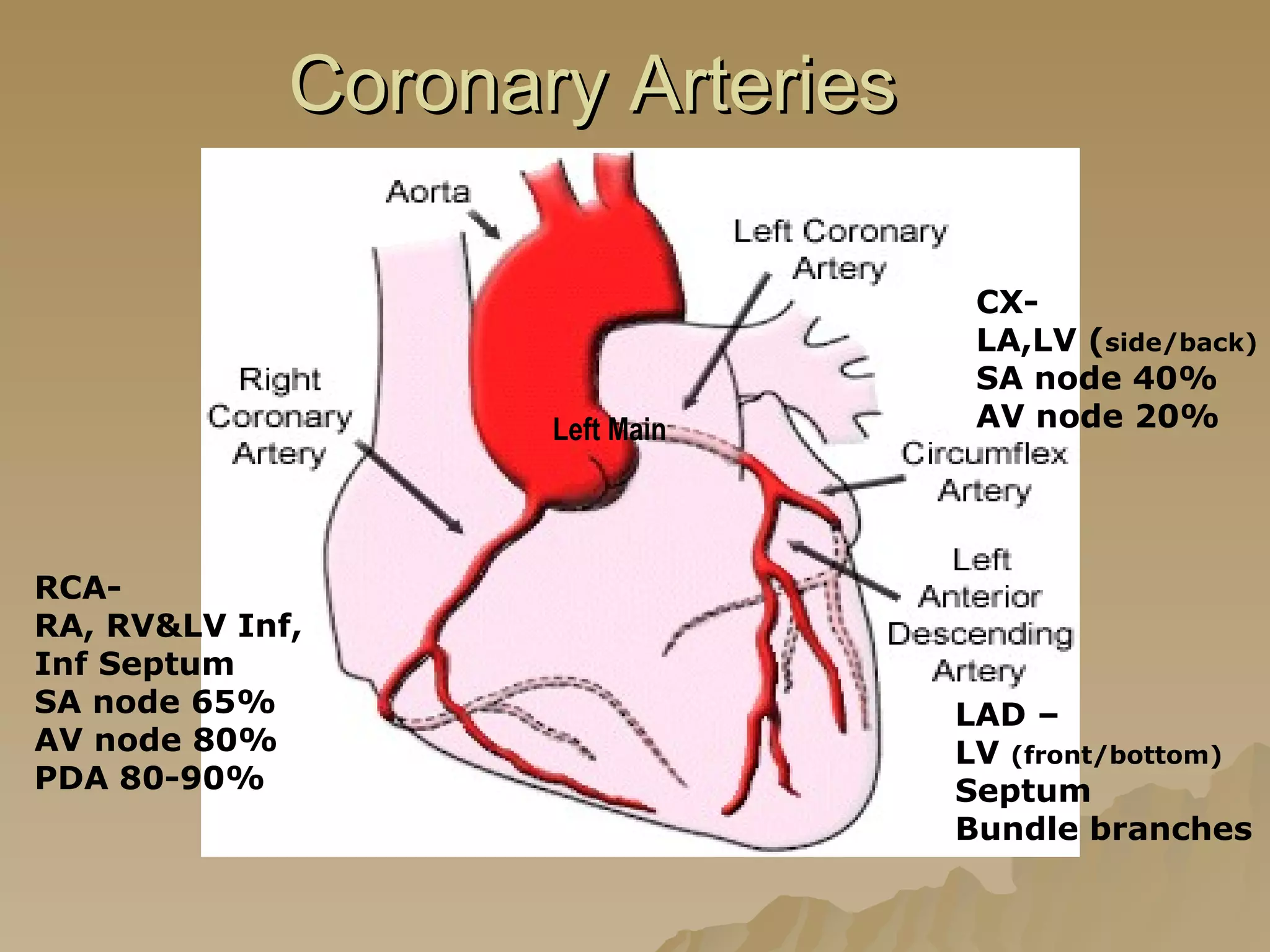
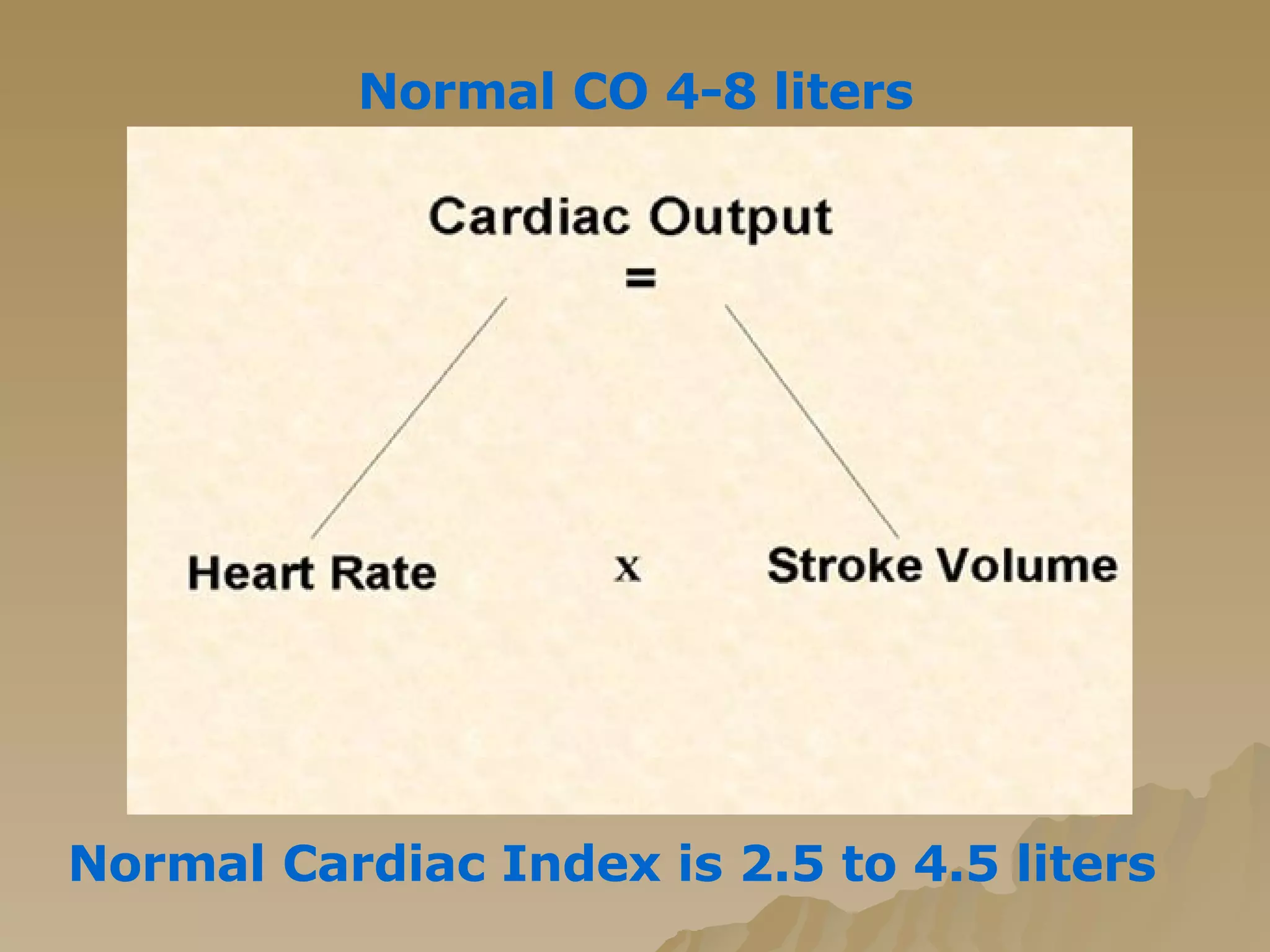
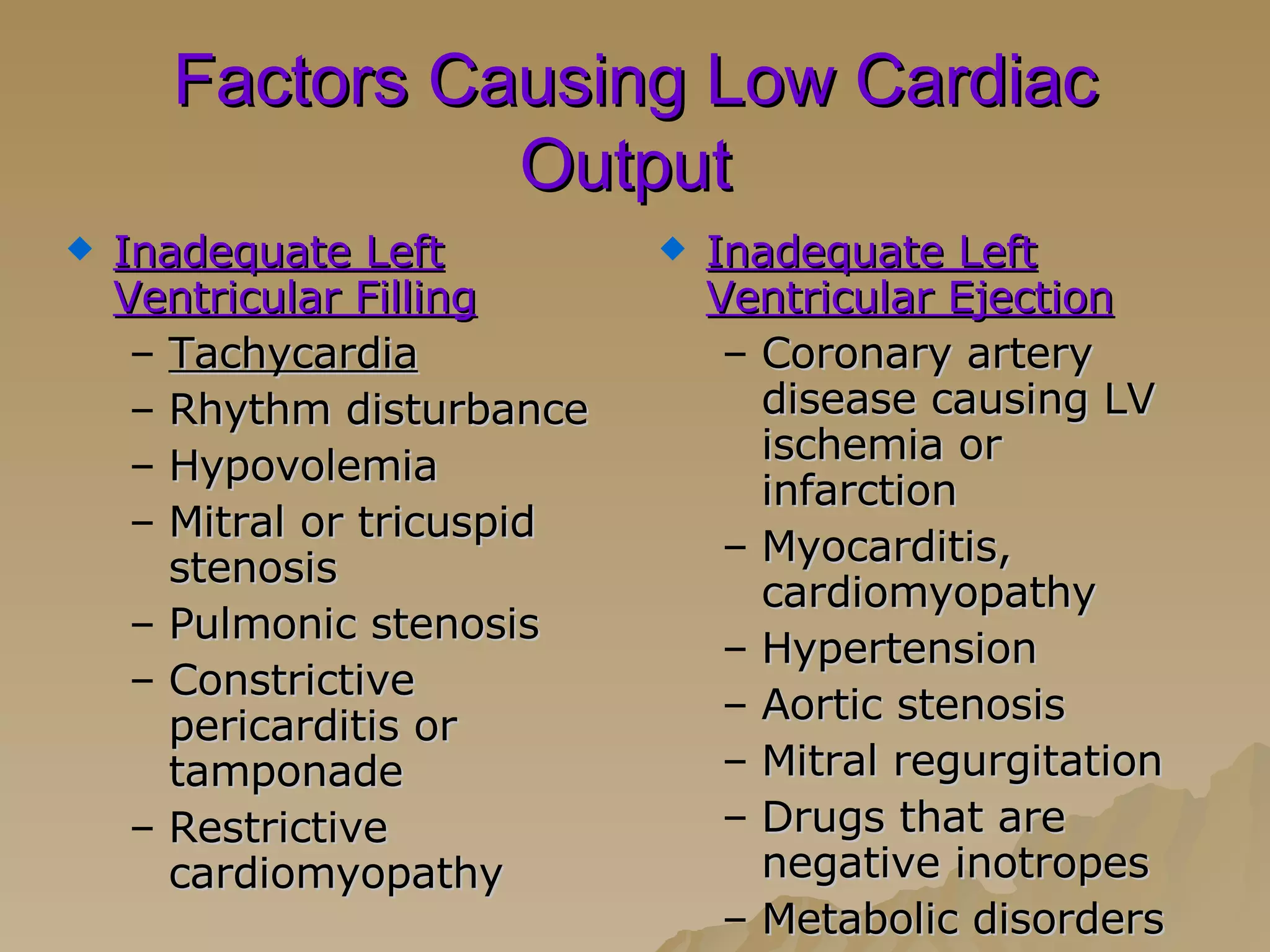
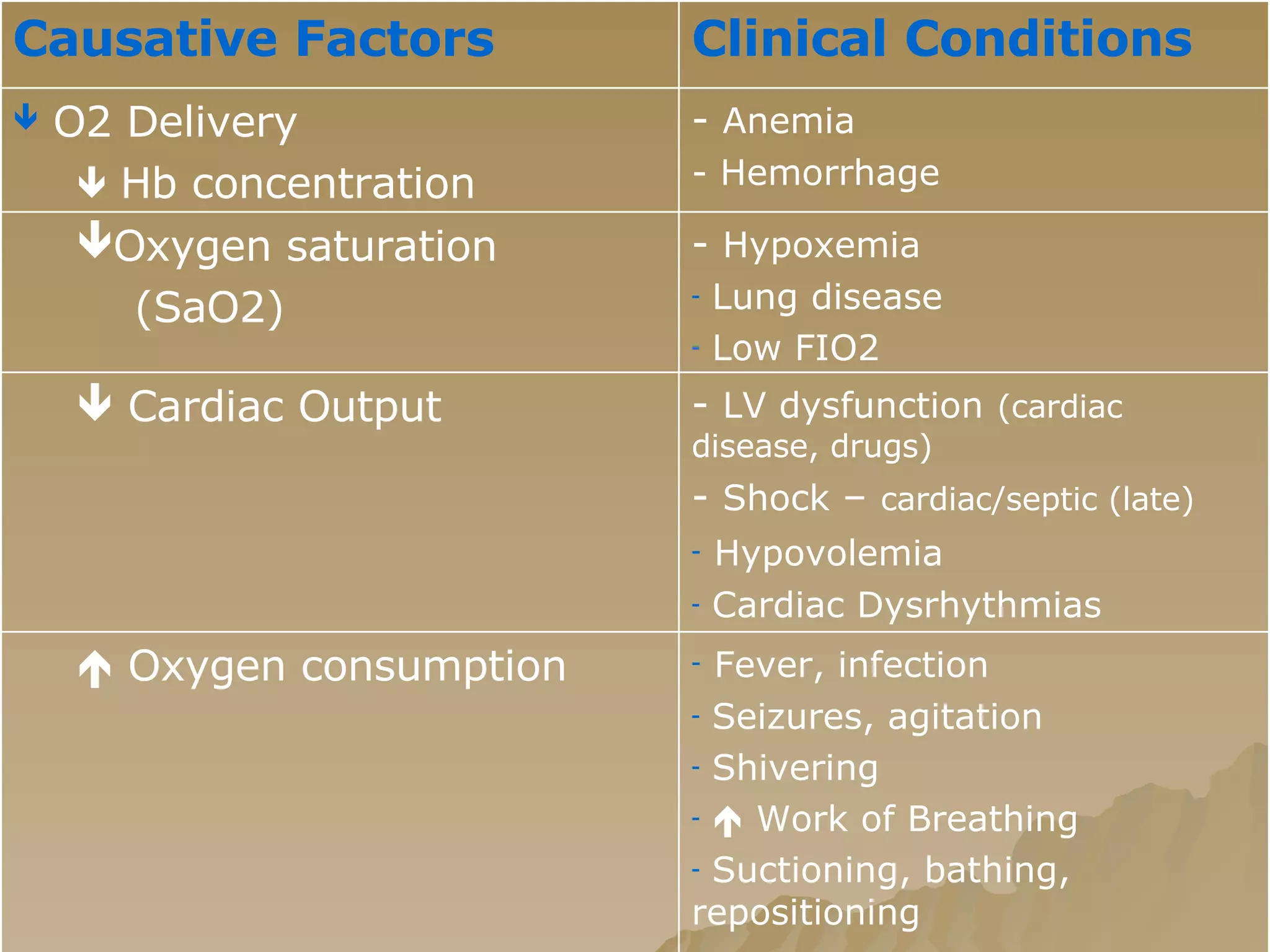
2. Indications for hemodynamic monitoring include decreased cardiac output from various causes, shock, loss of cardiac function, and coronary artery disease.
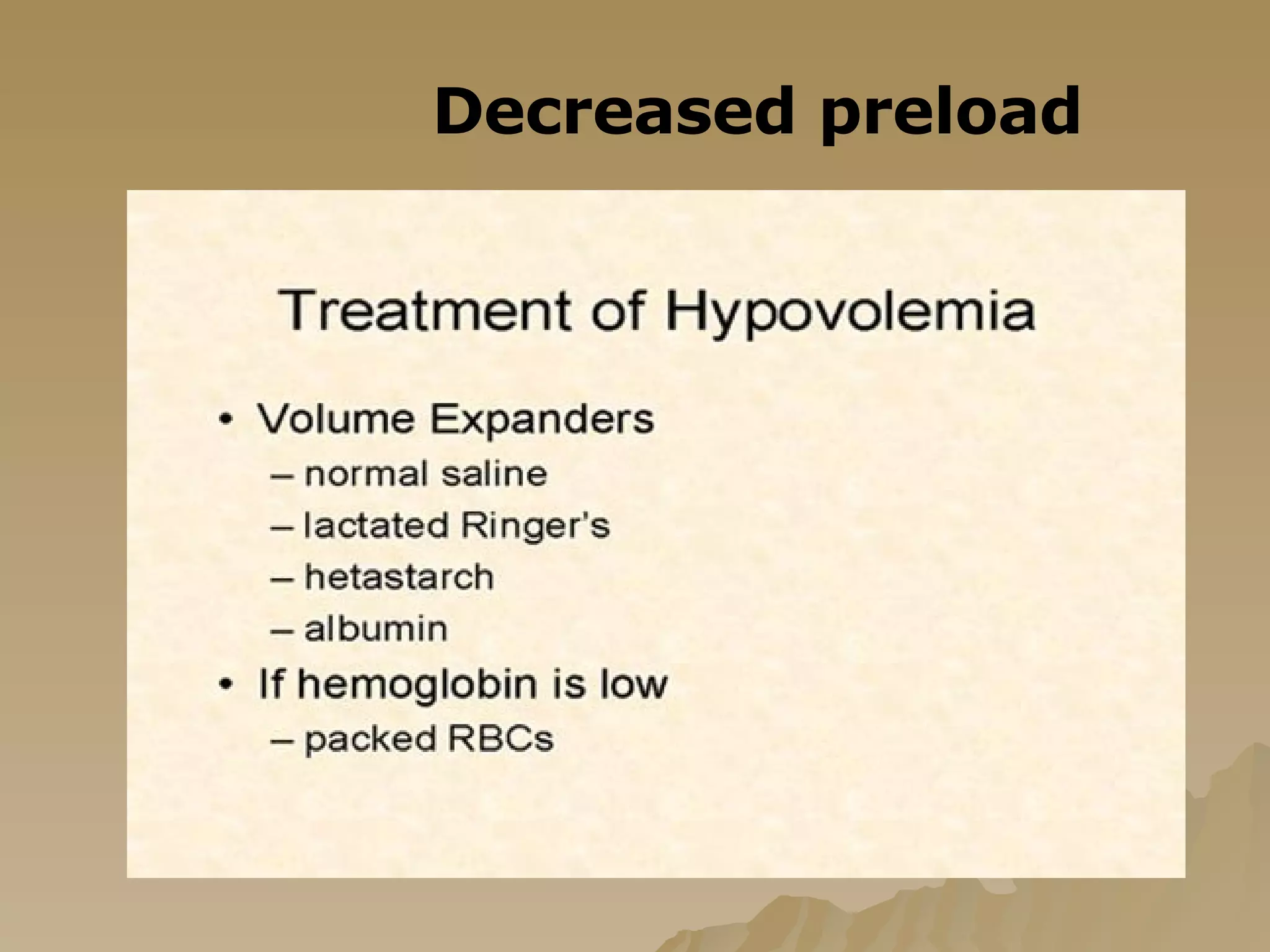
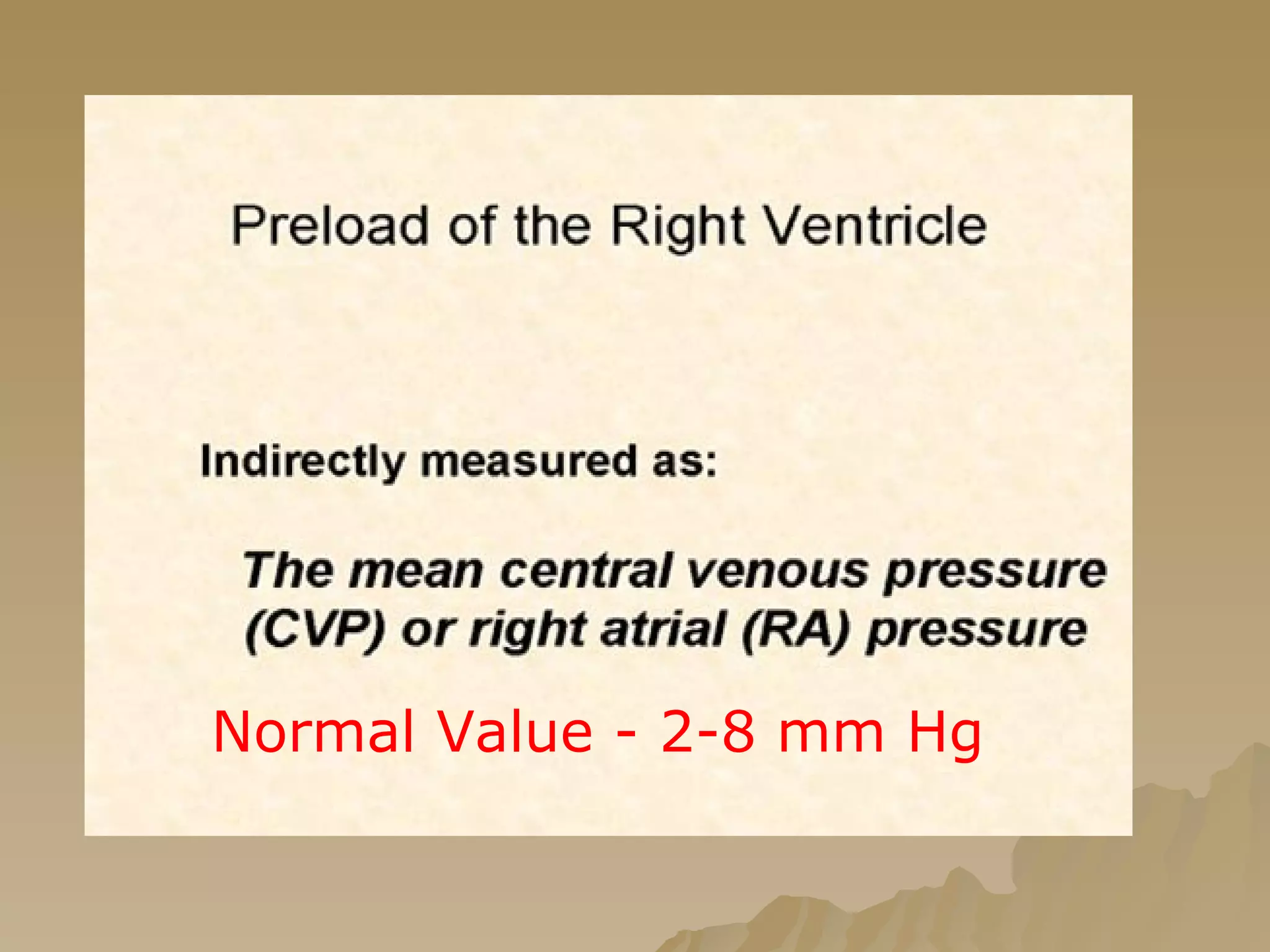
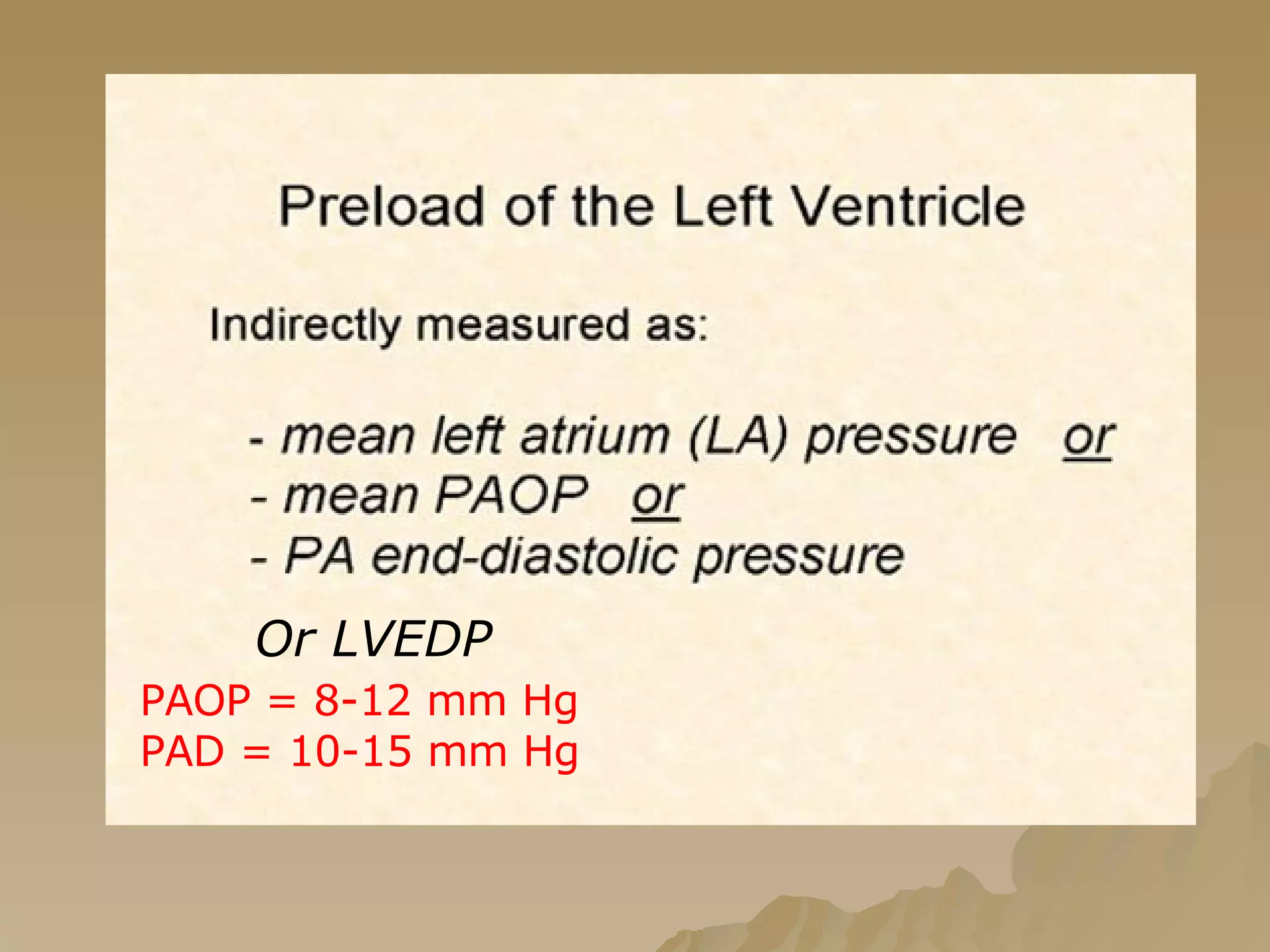
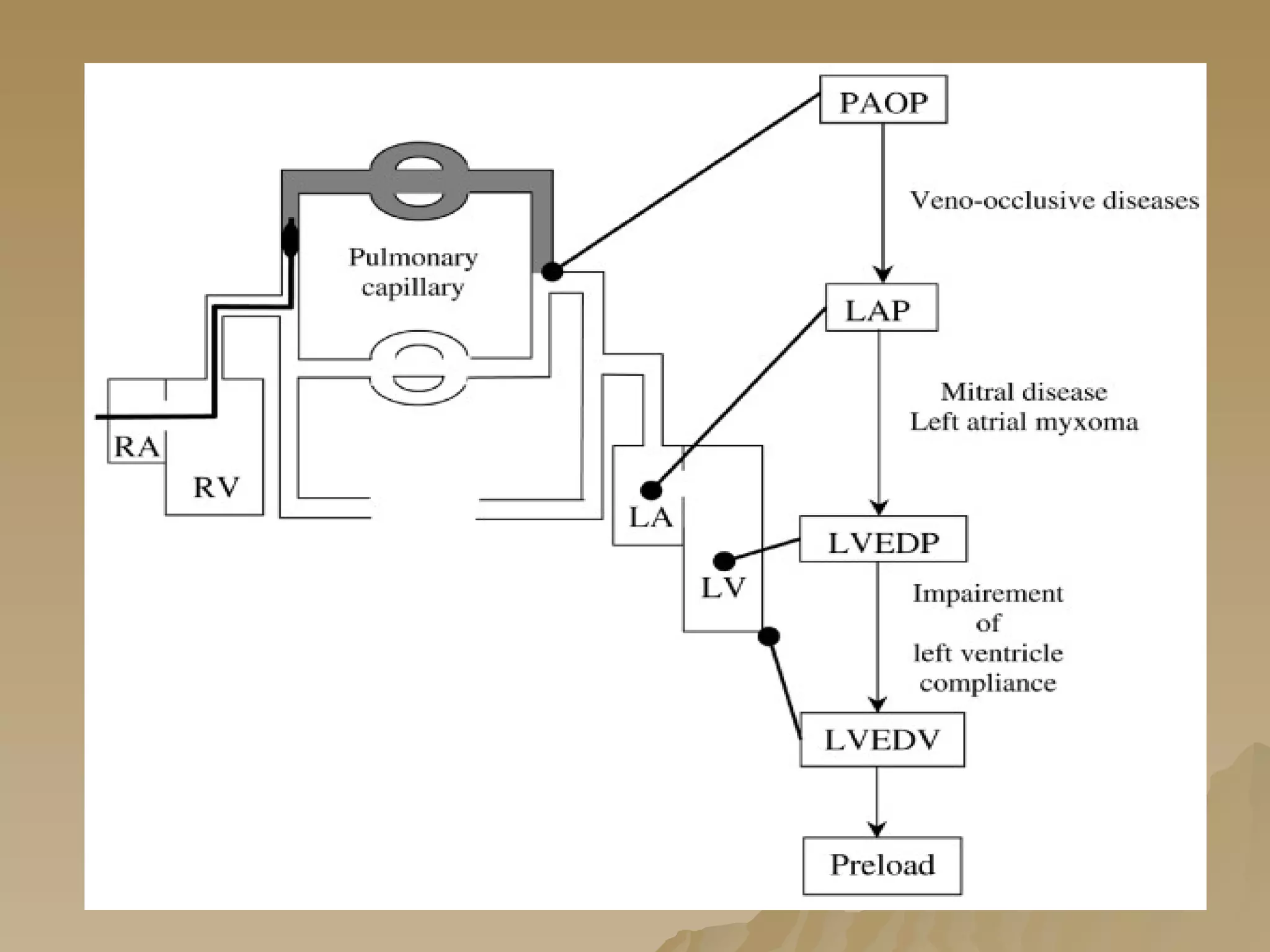
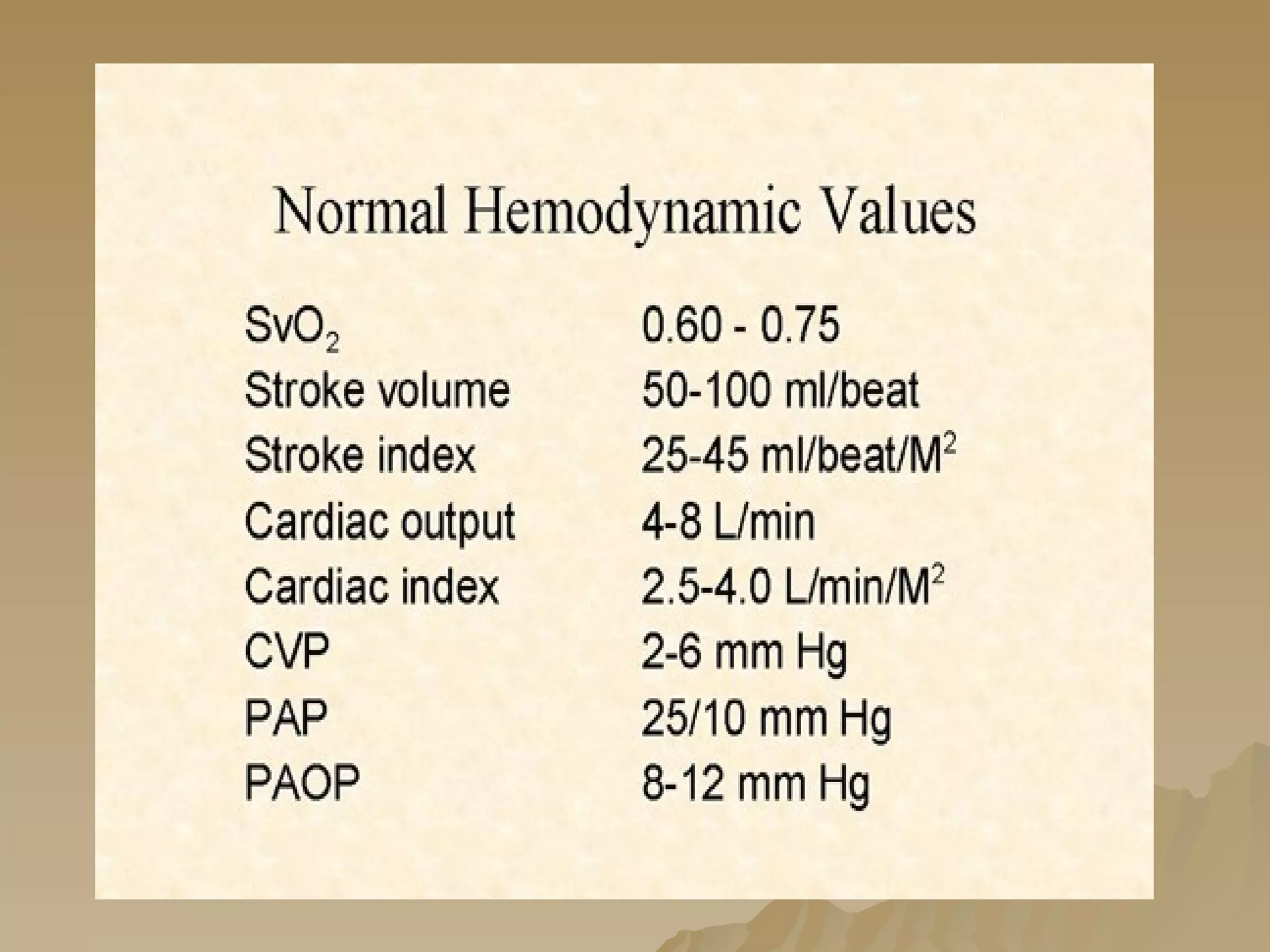
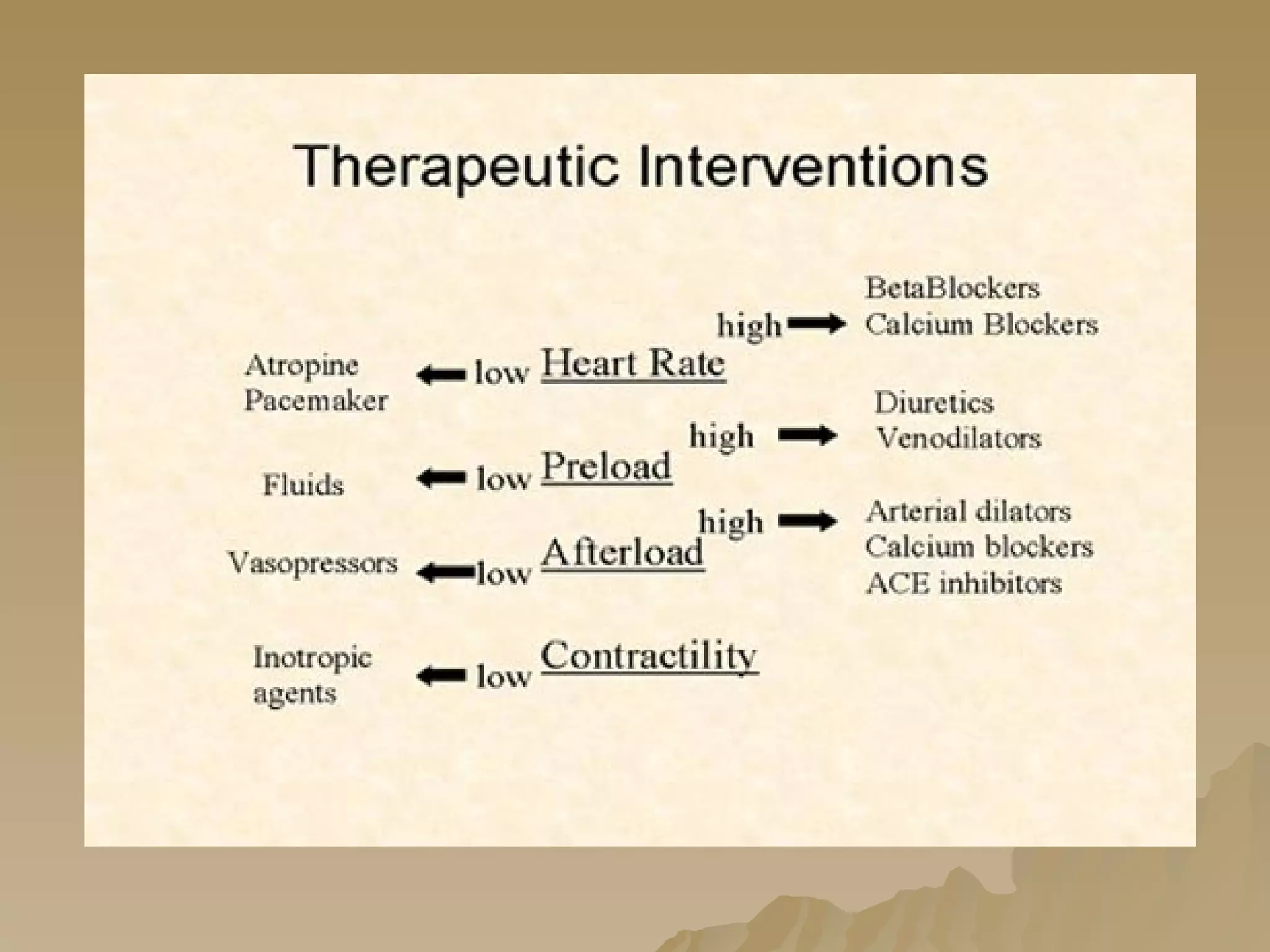
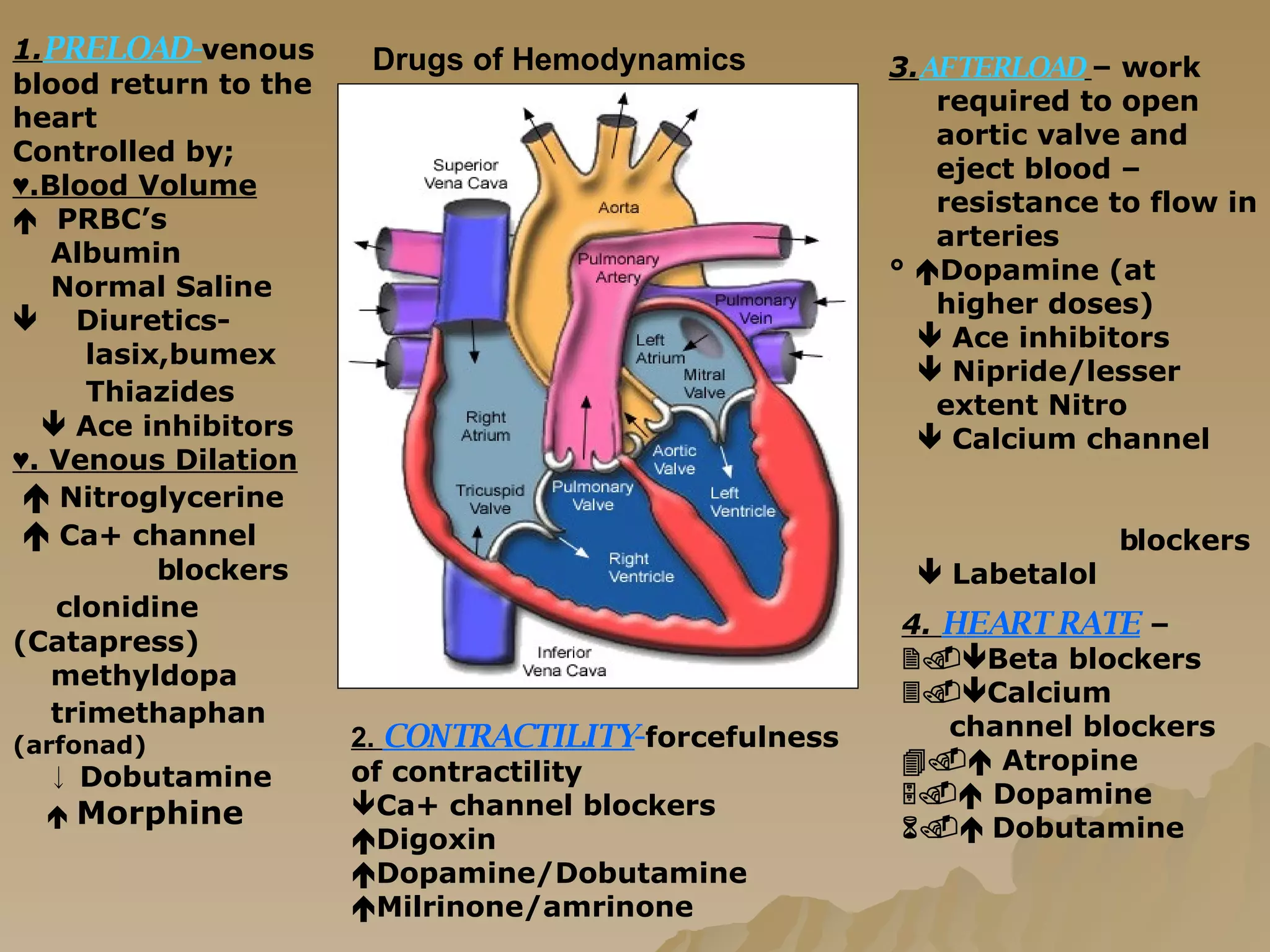
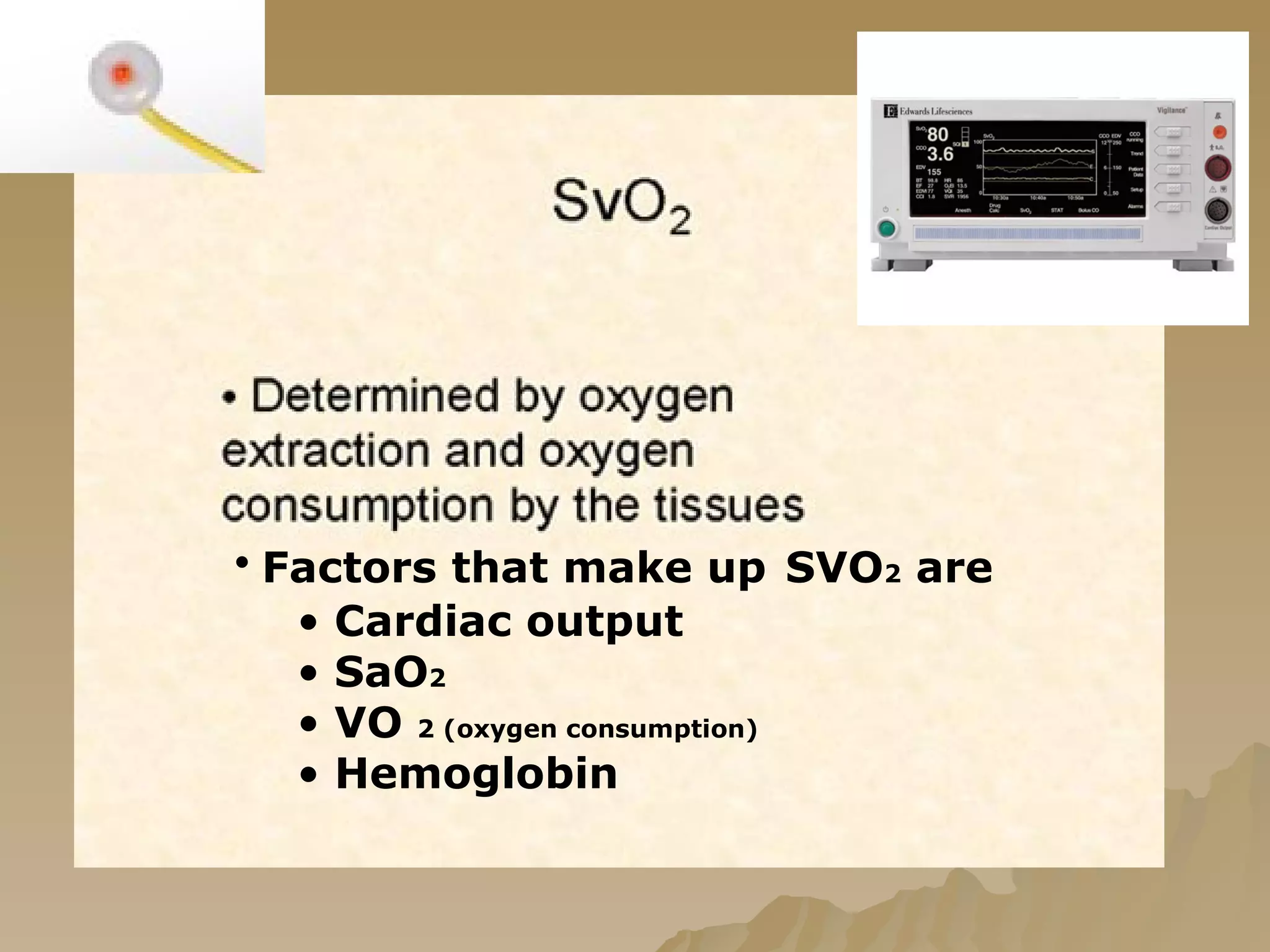
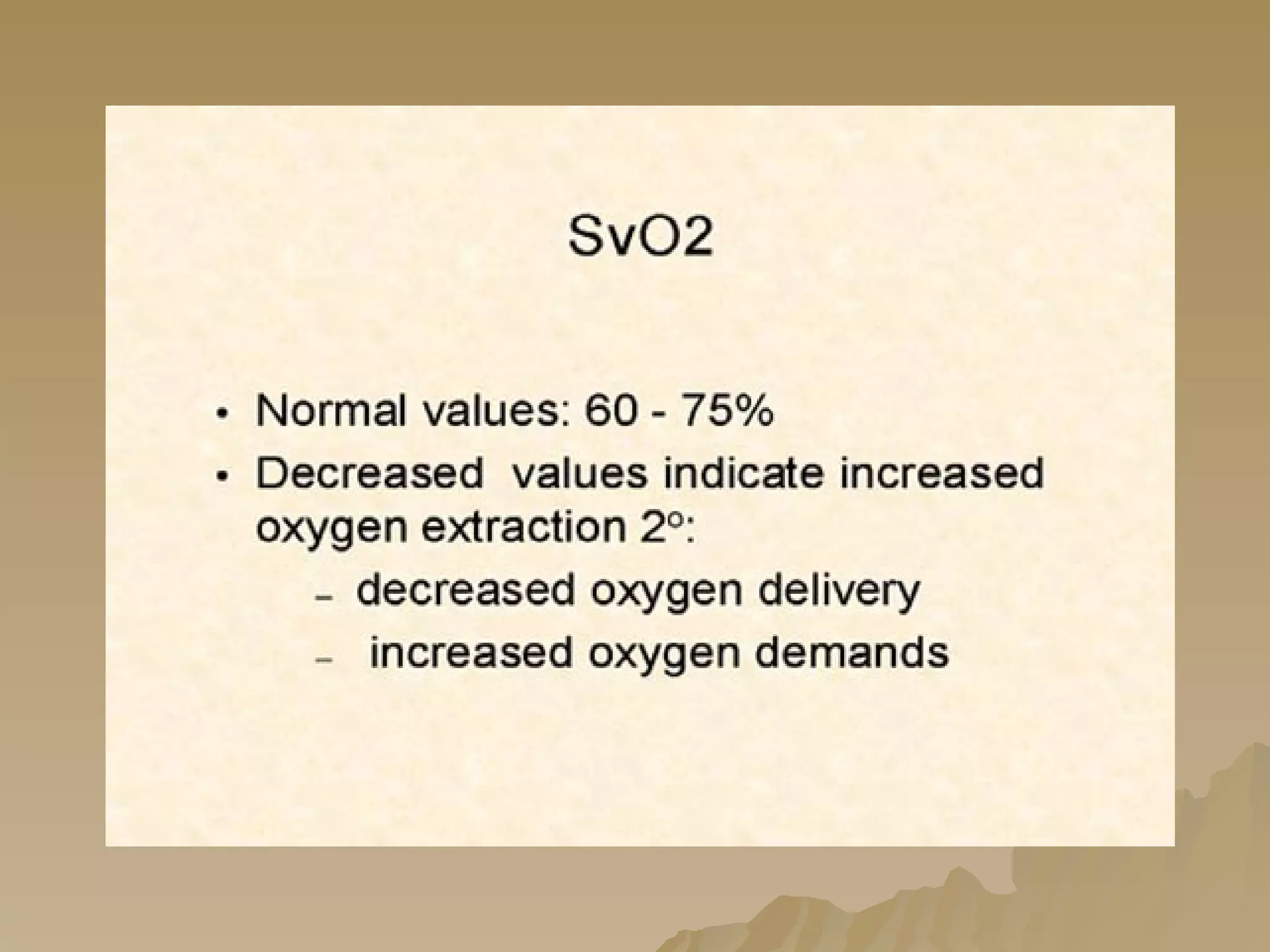
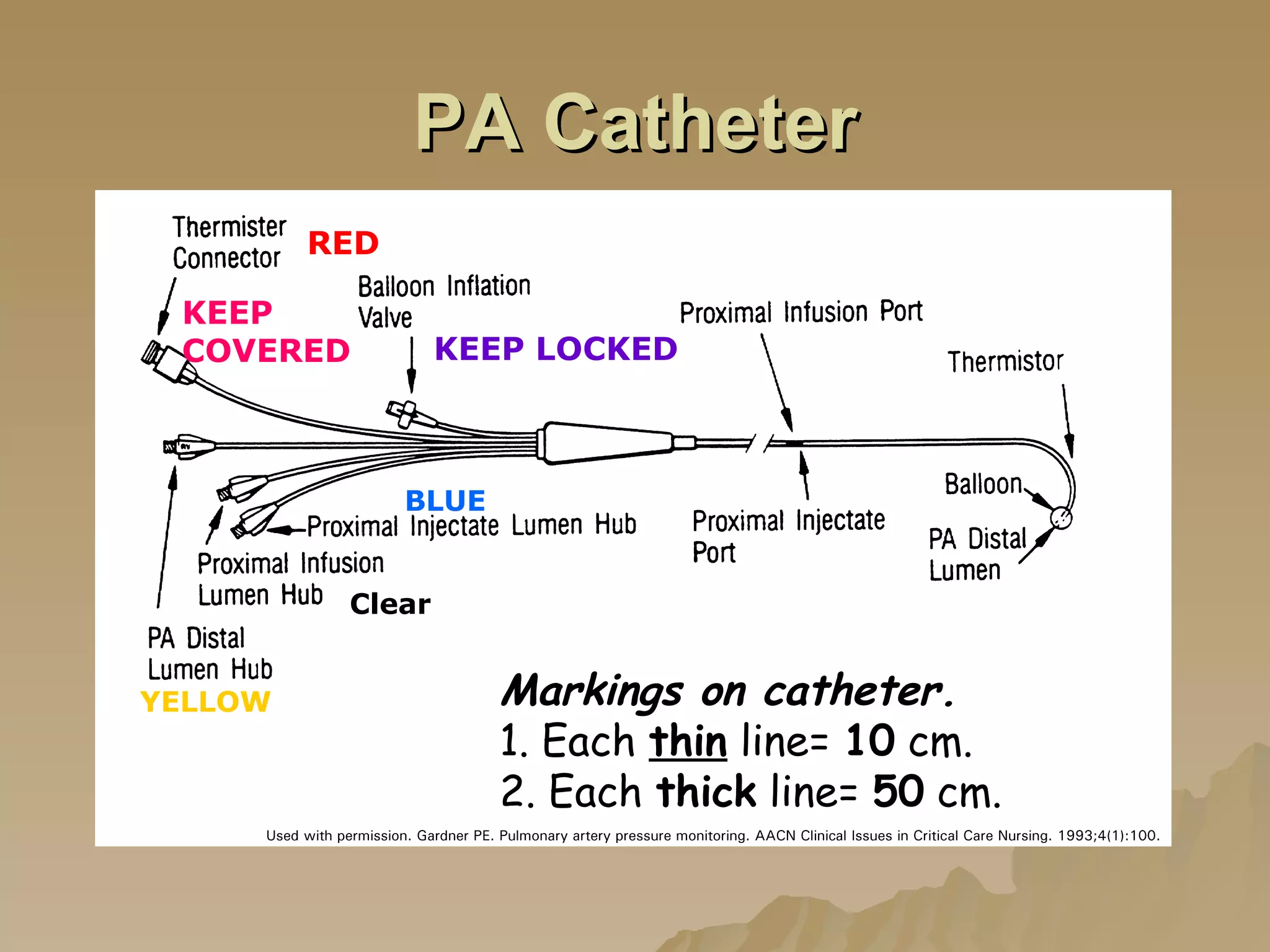
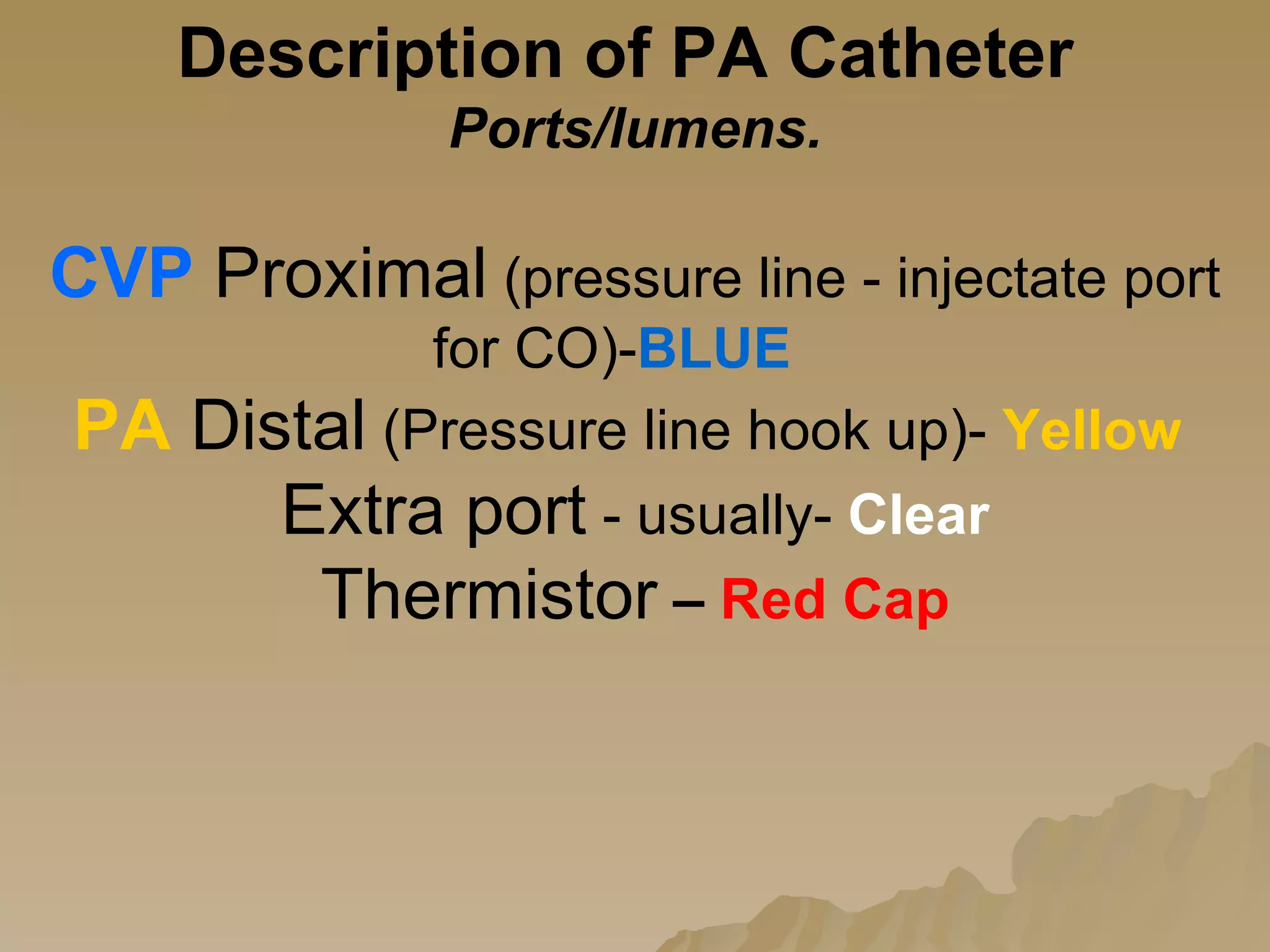
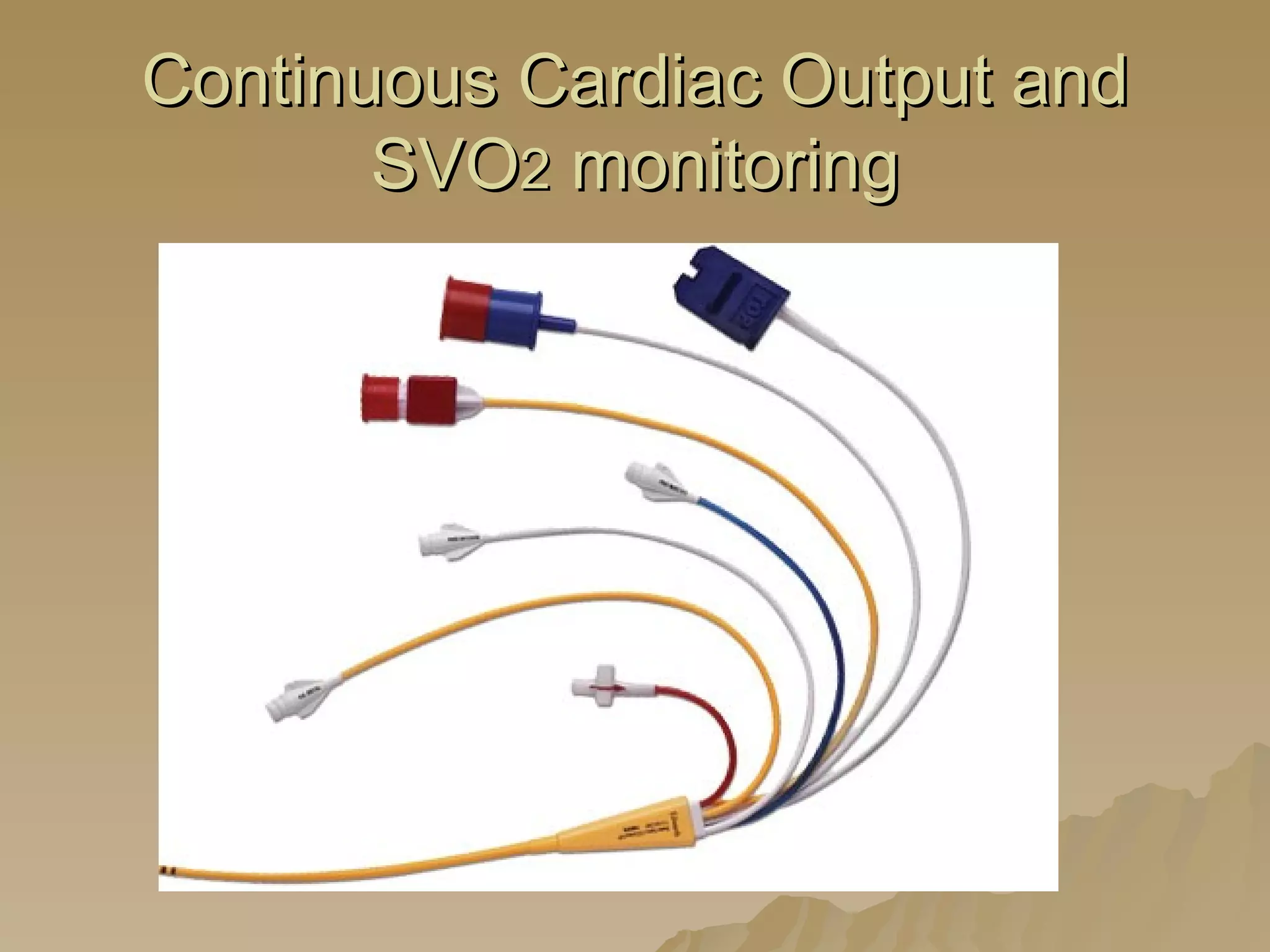
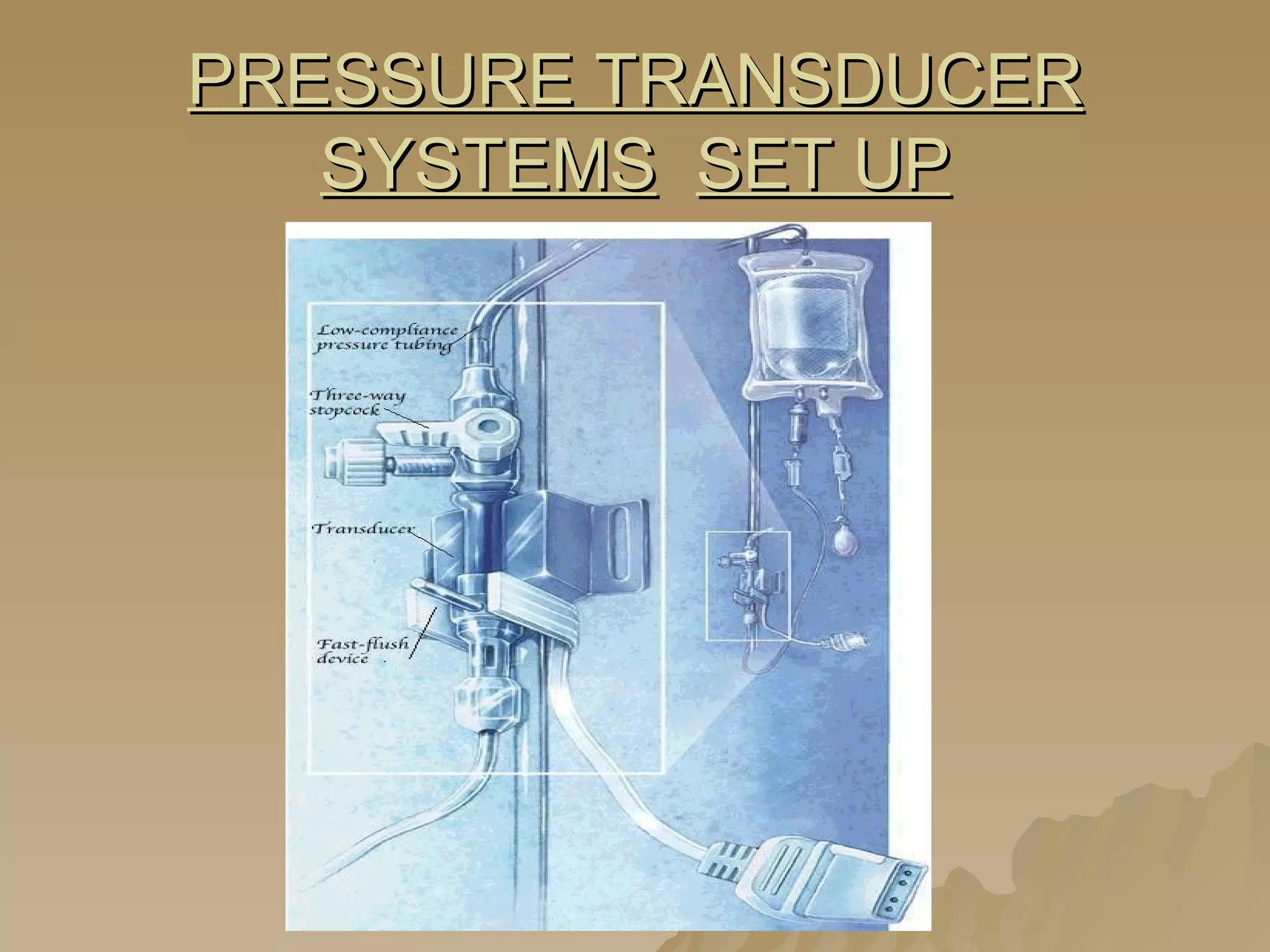
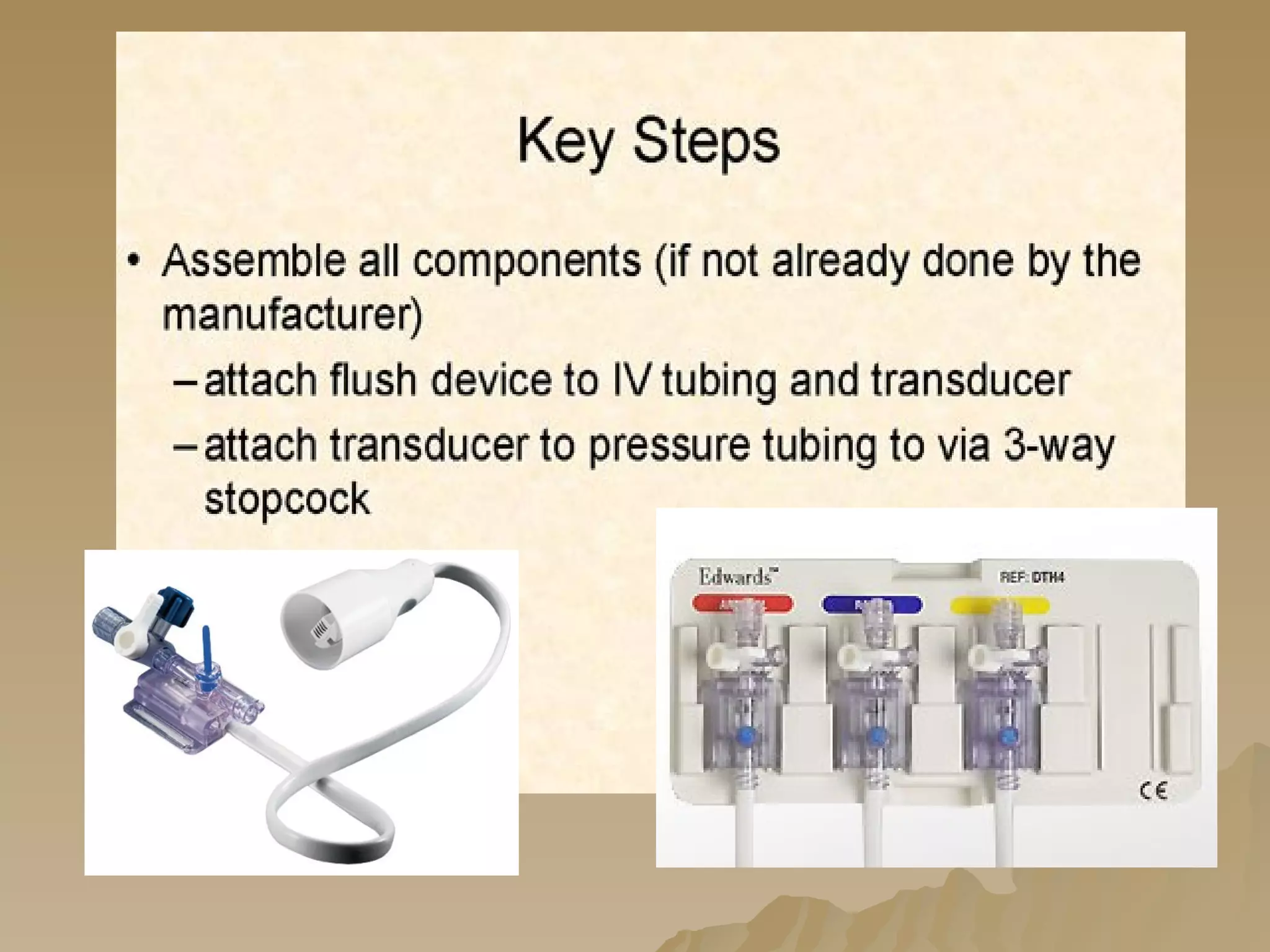
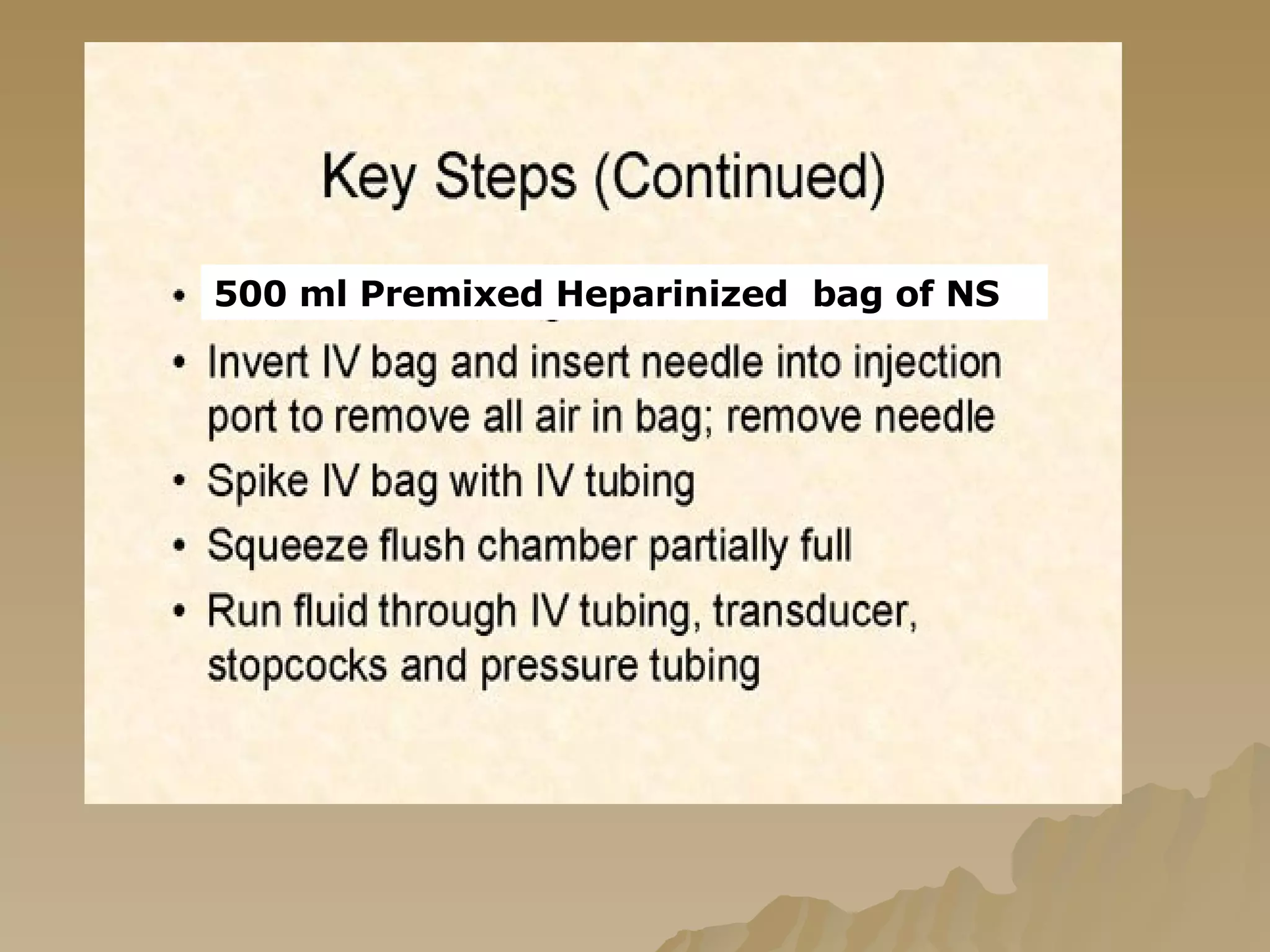
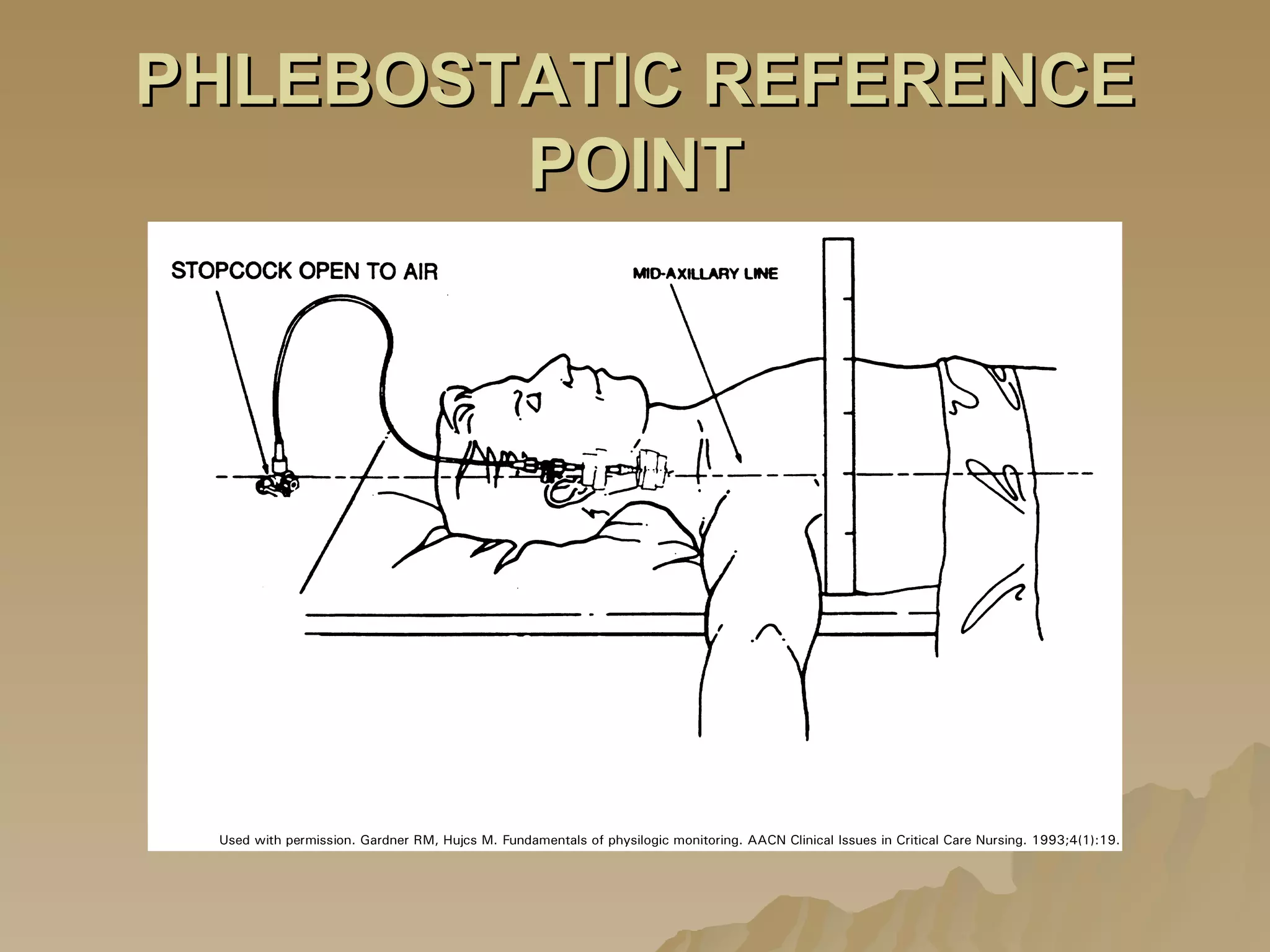
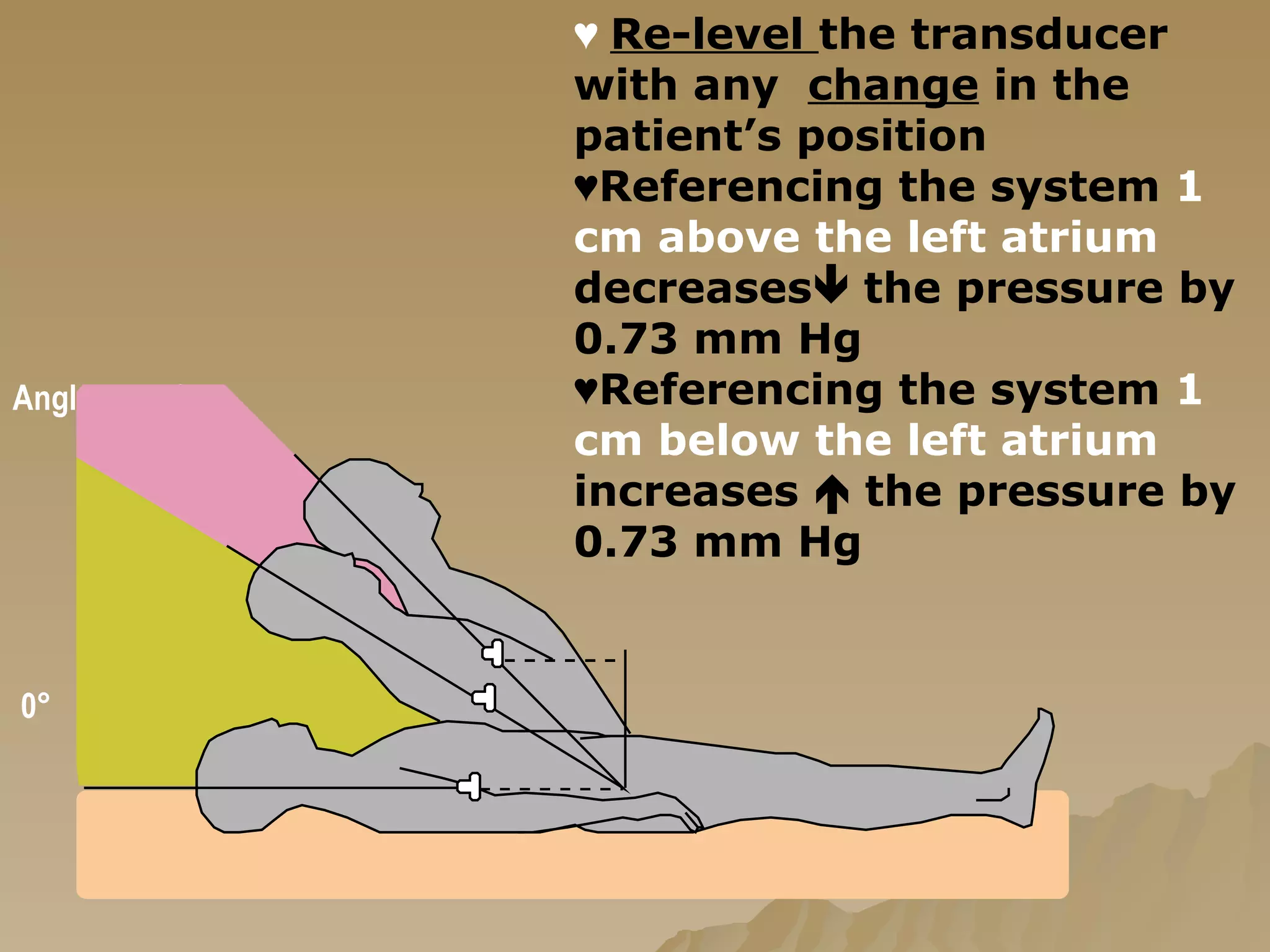
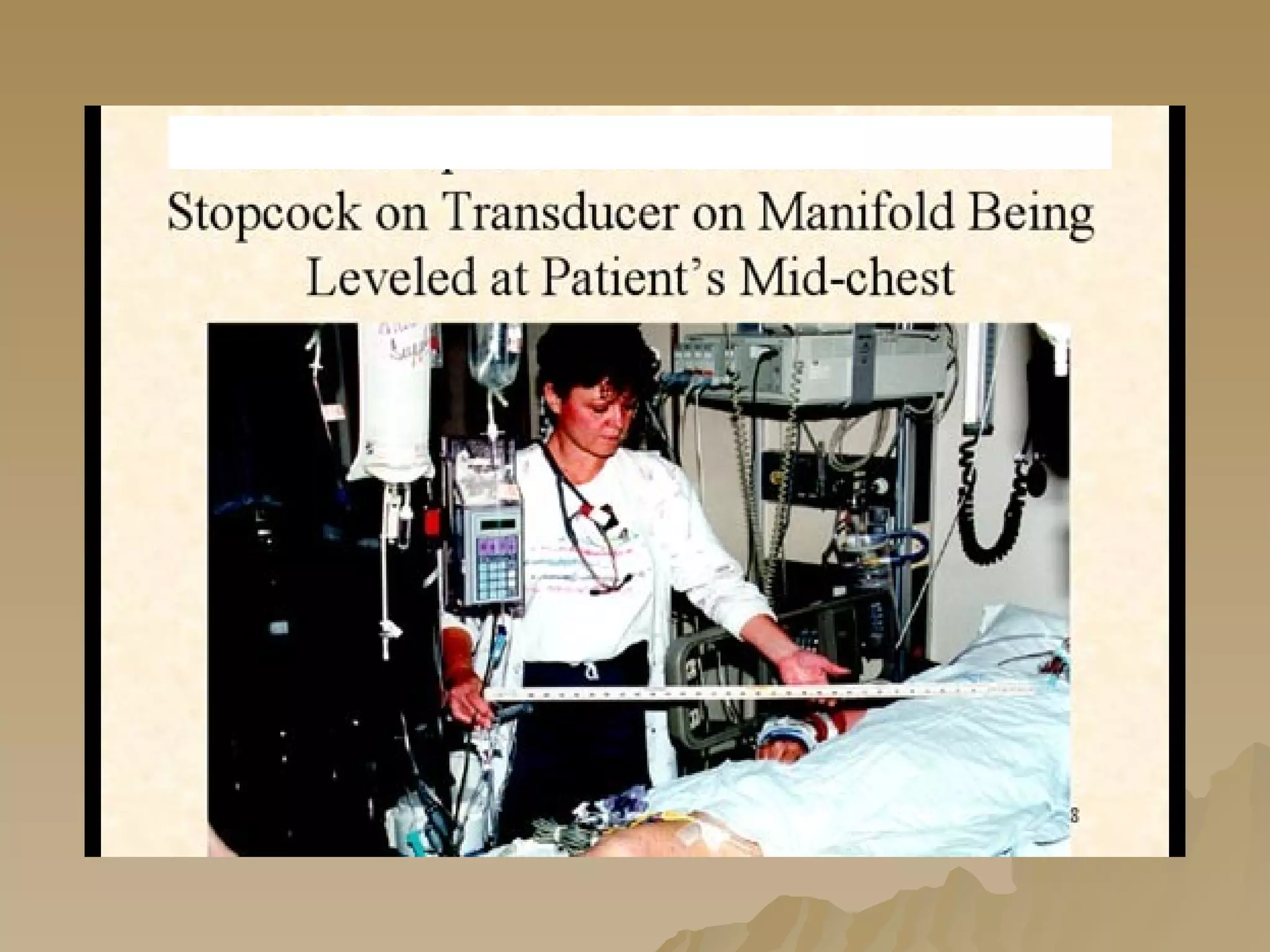
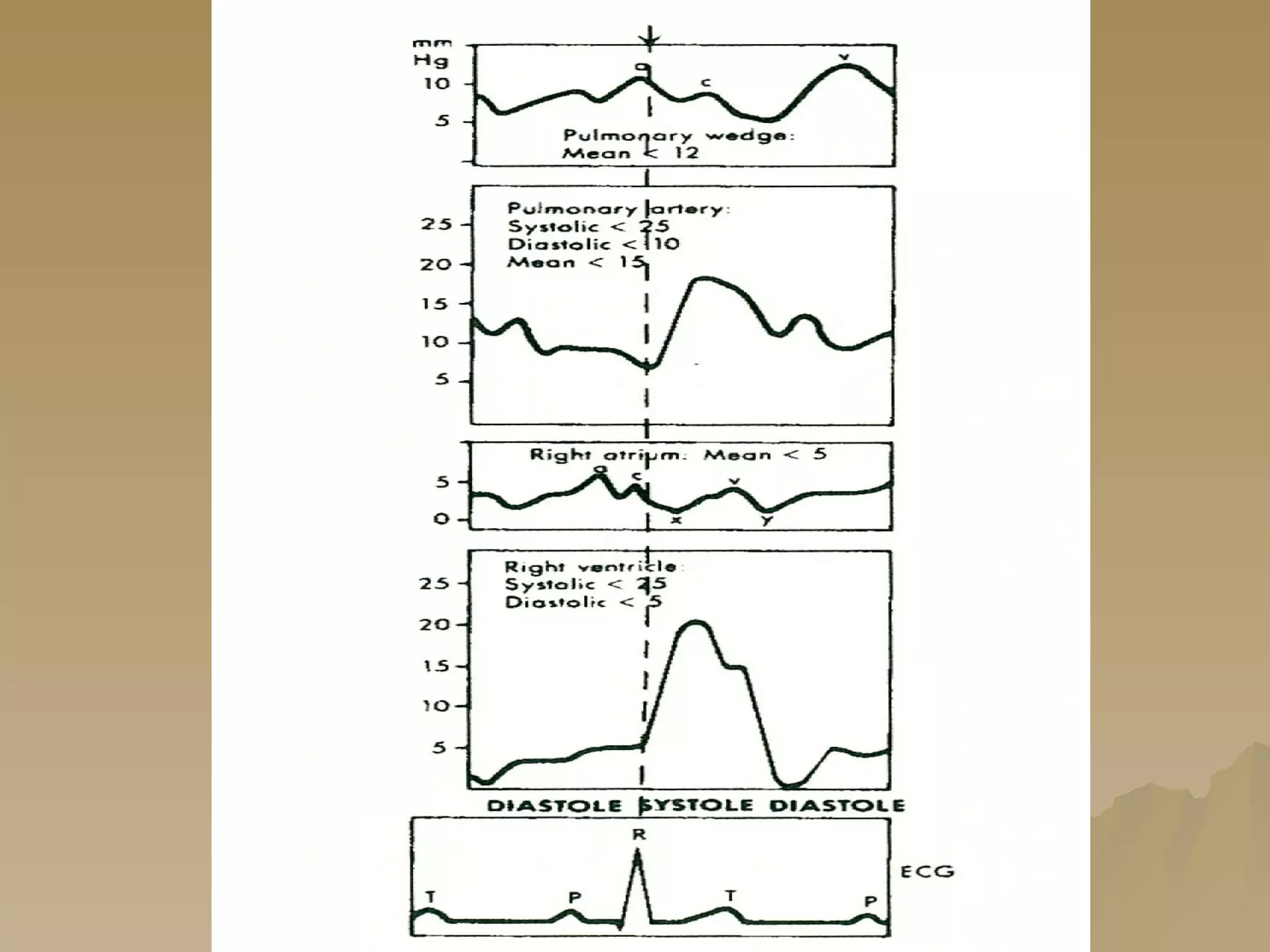
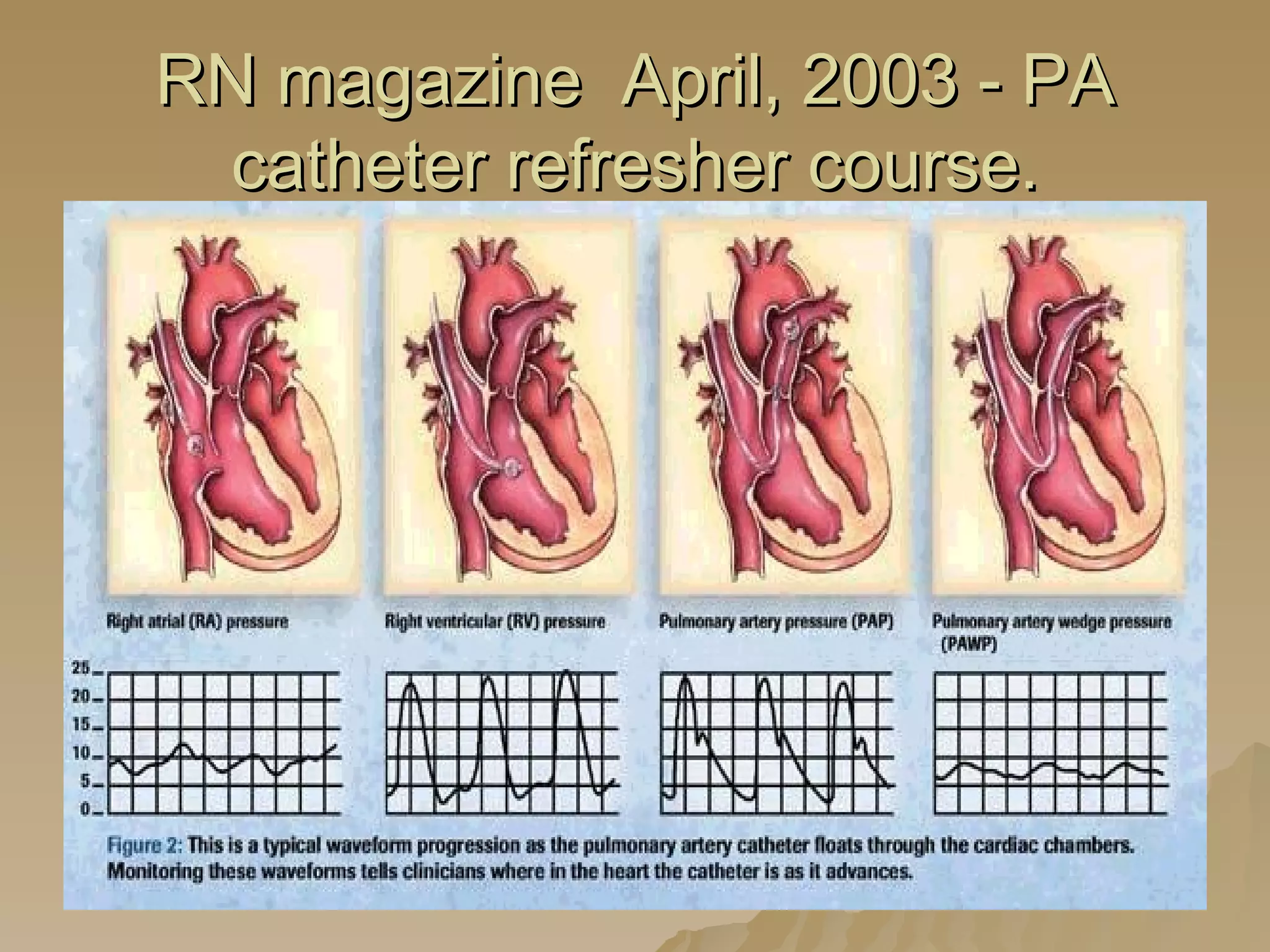
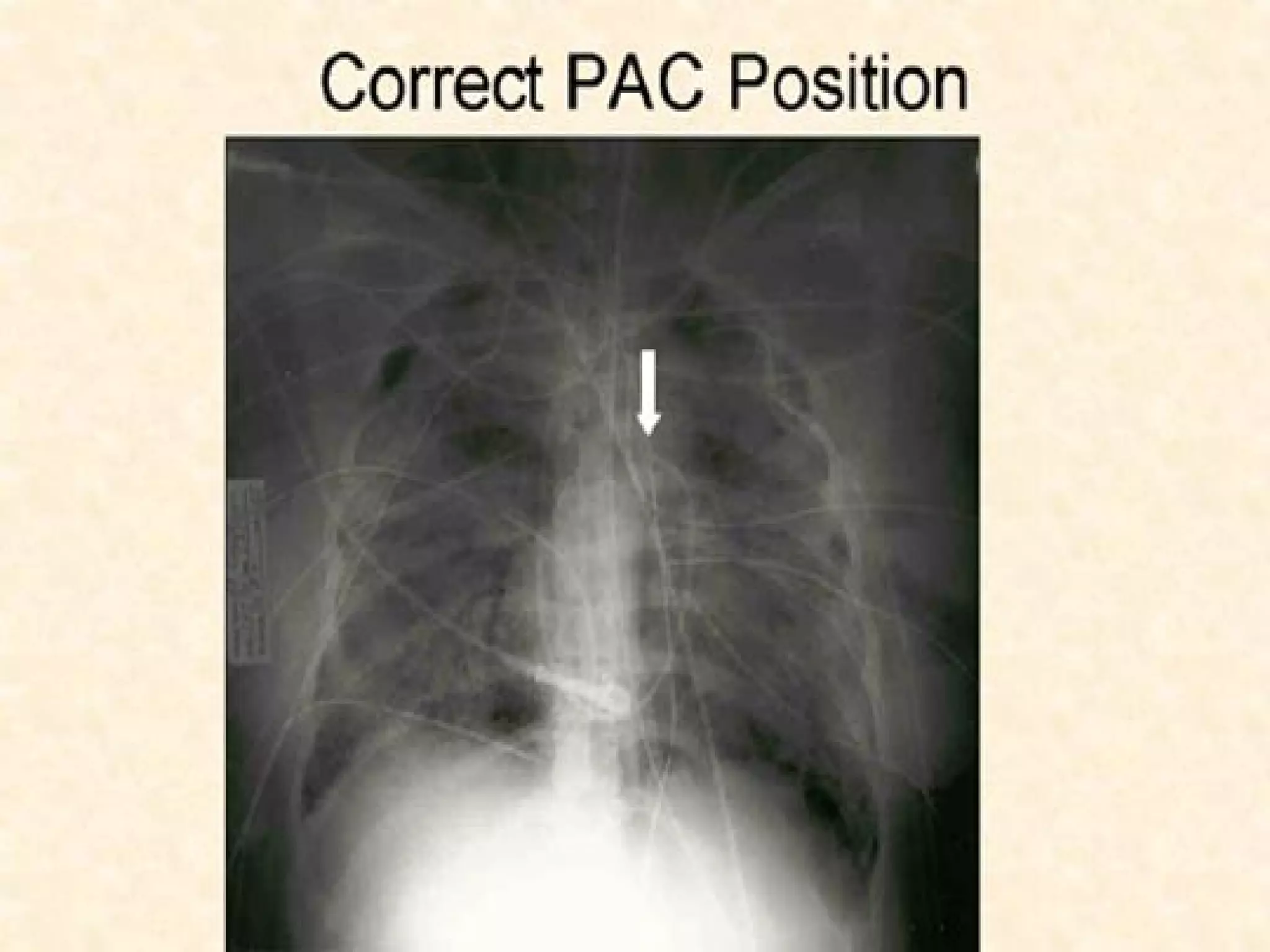
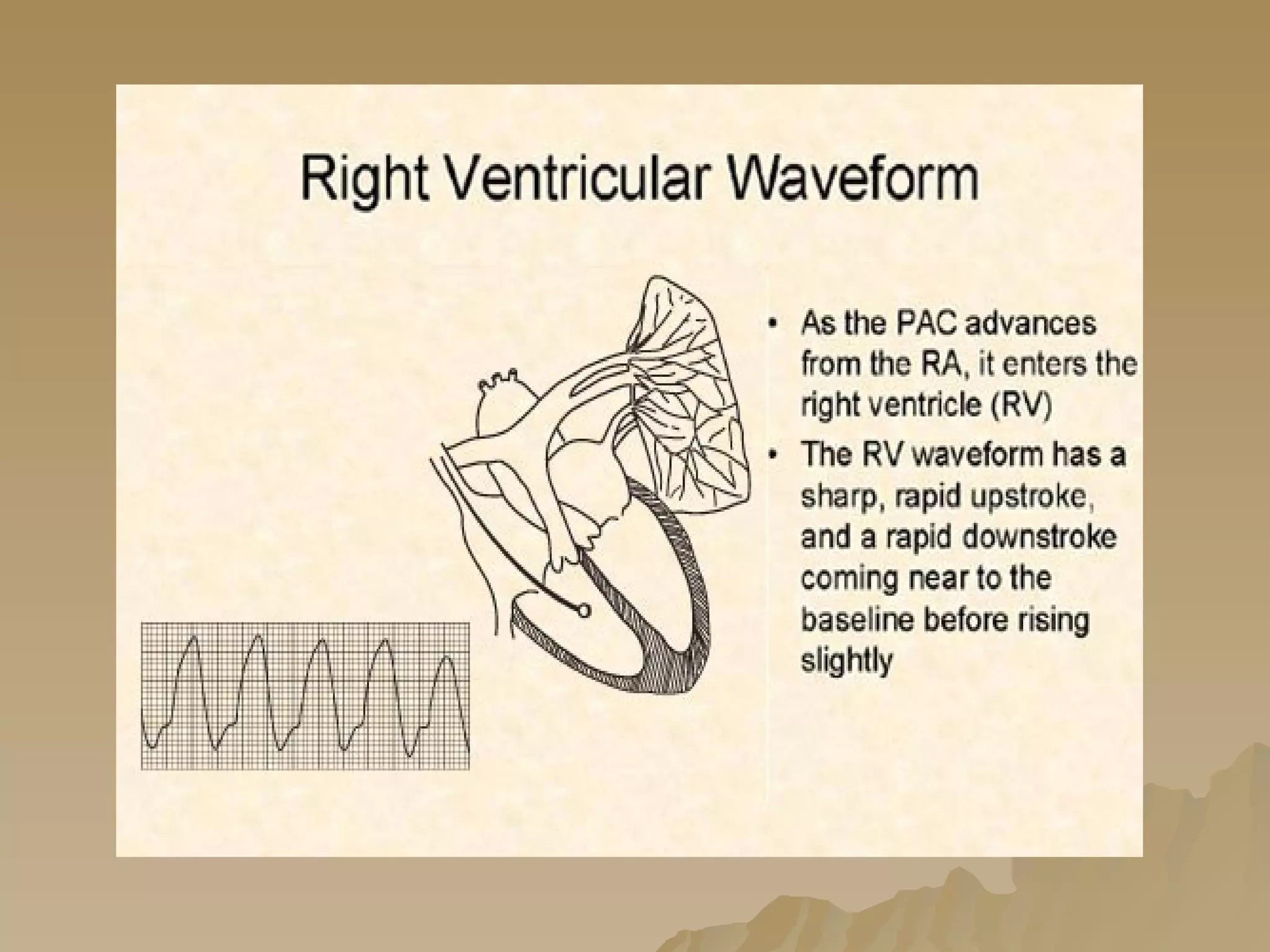
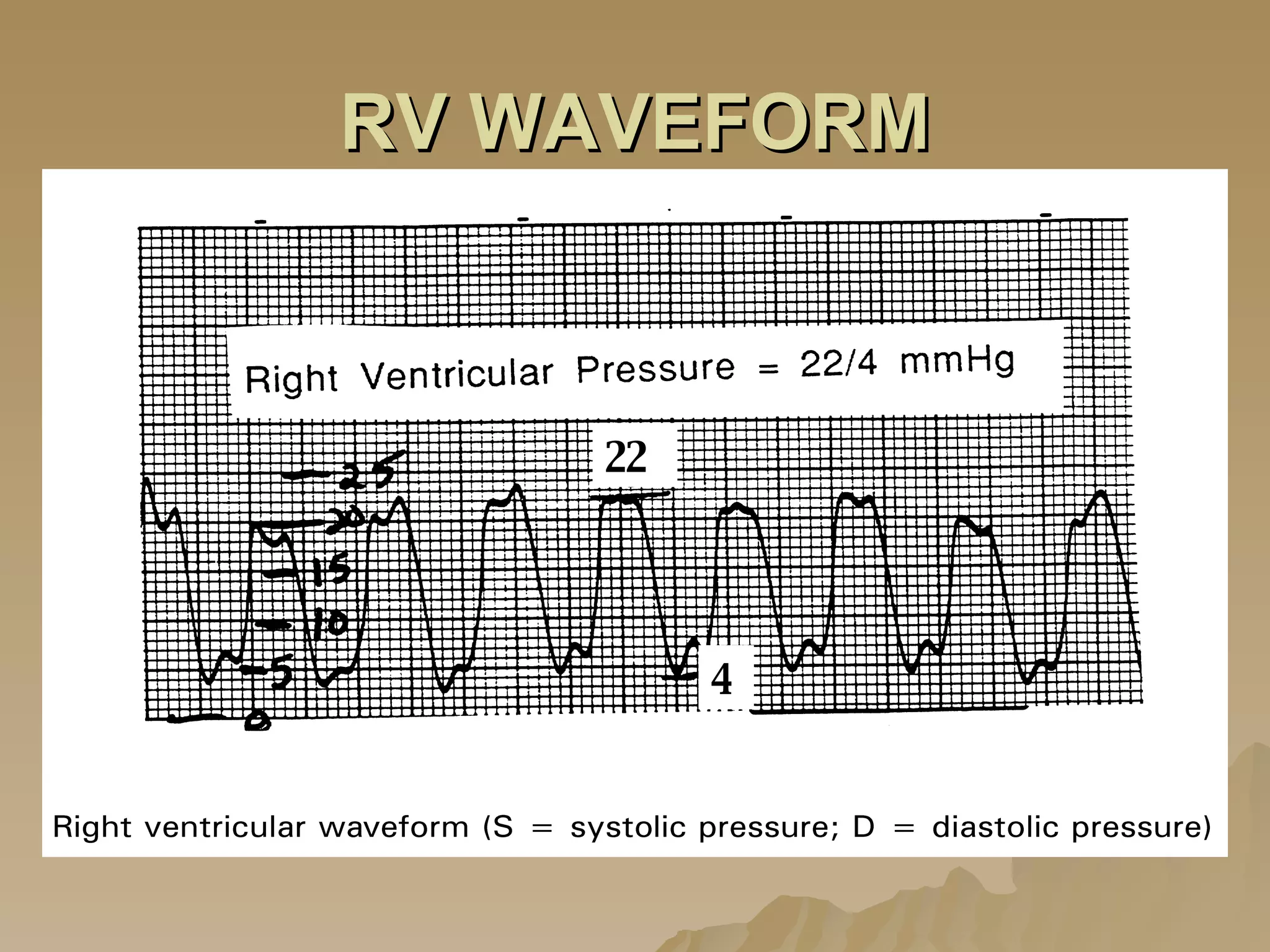
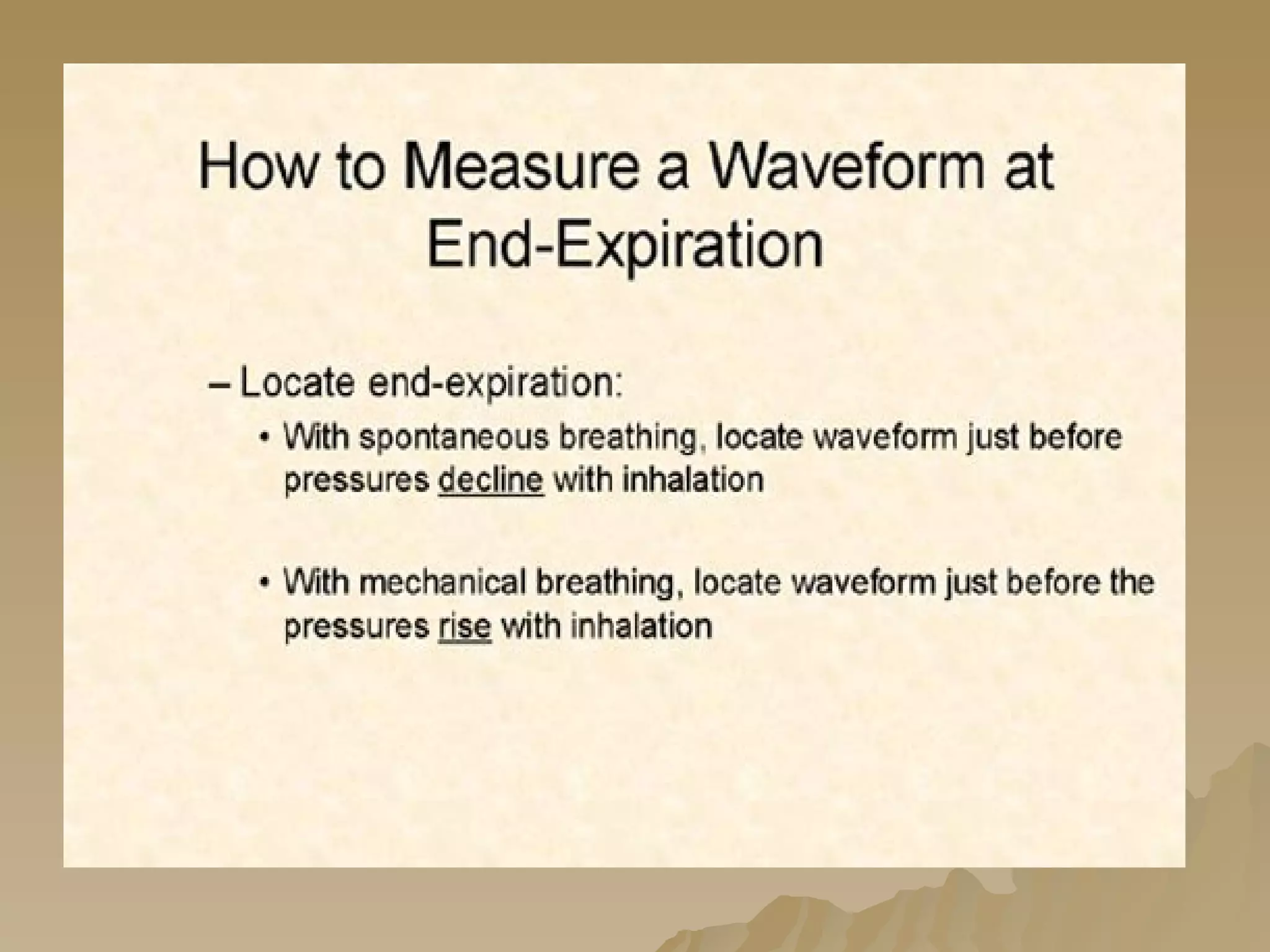
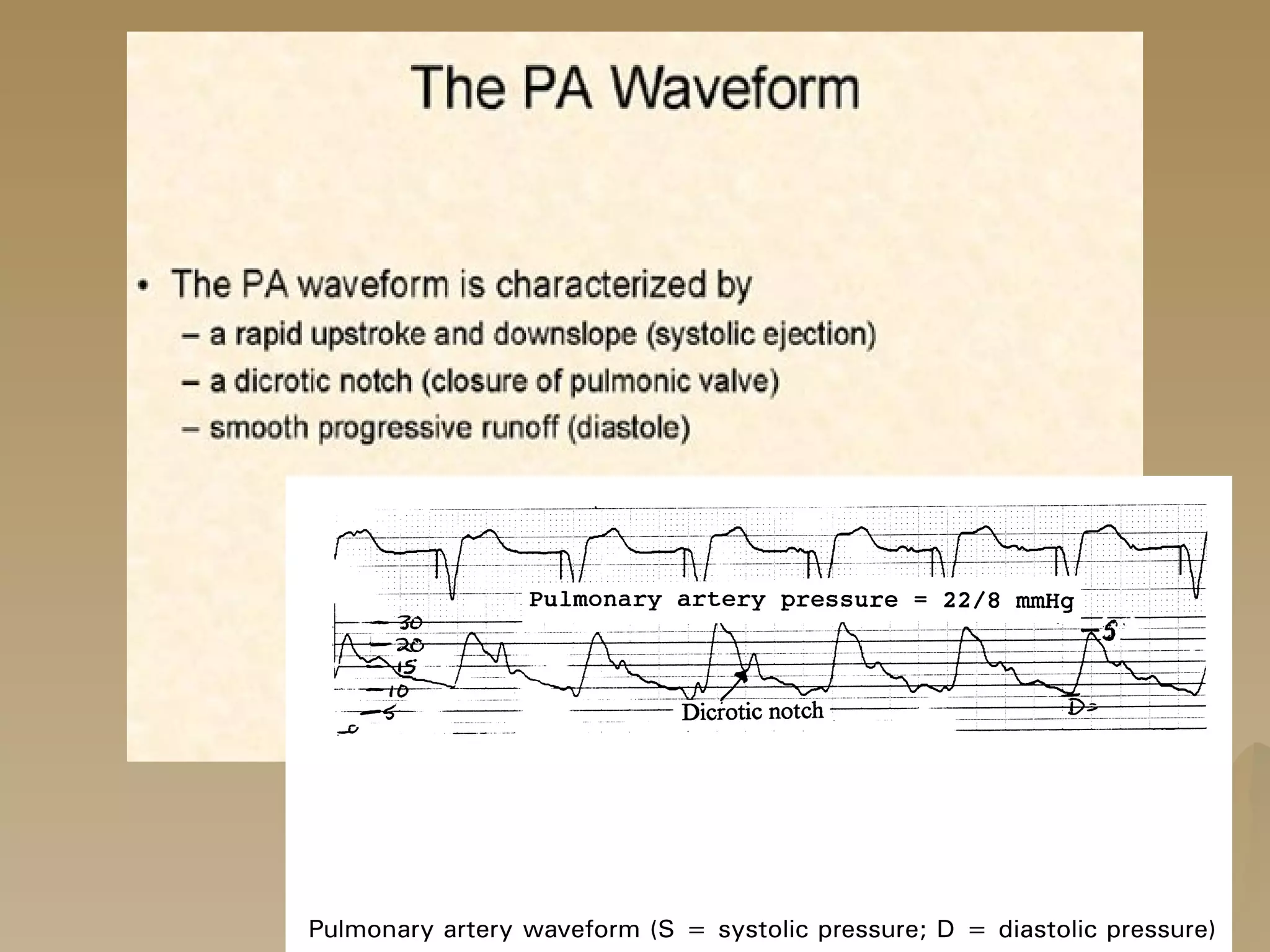
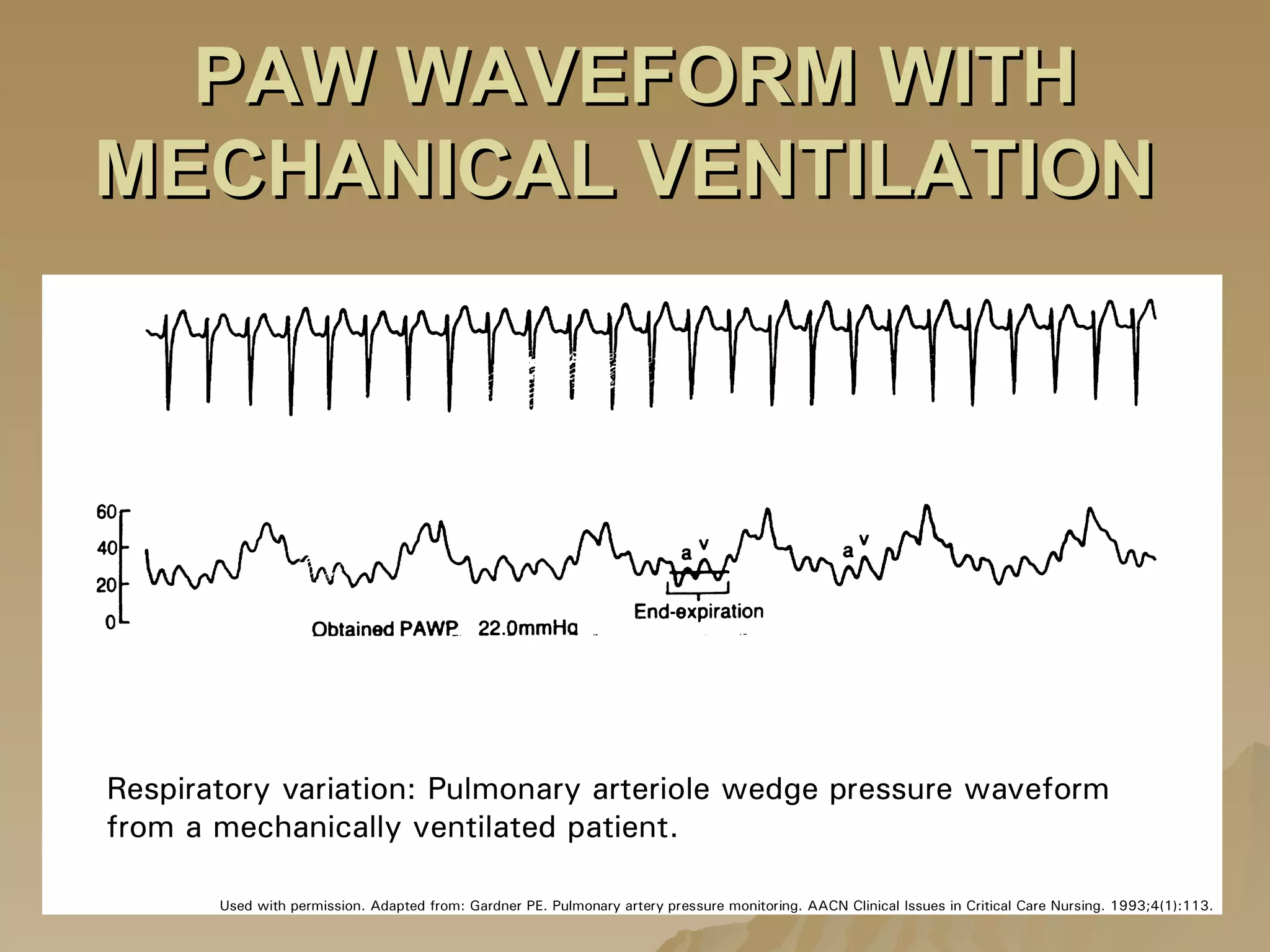
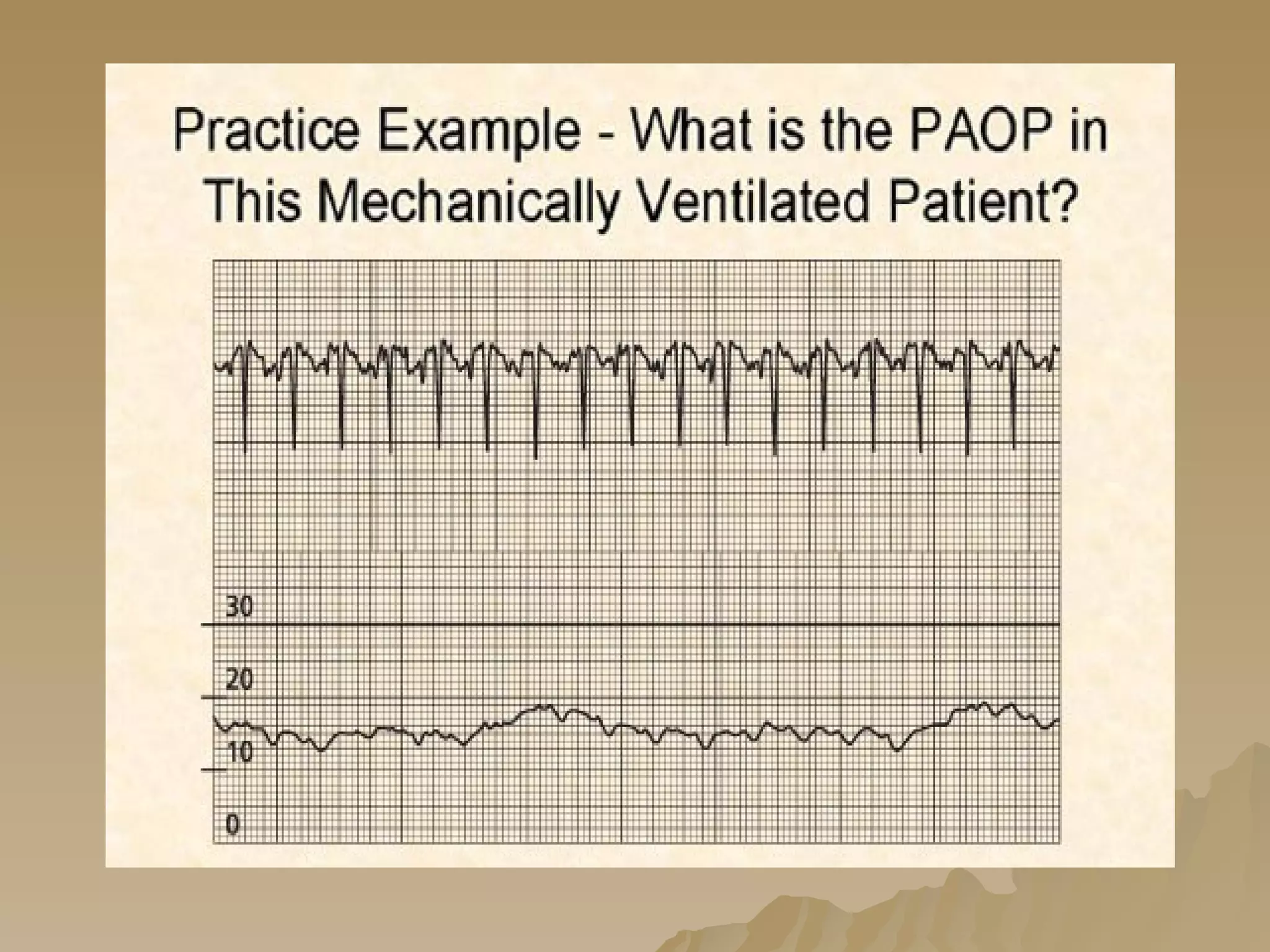
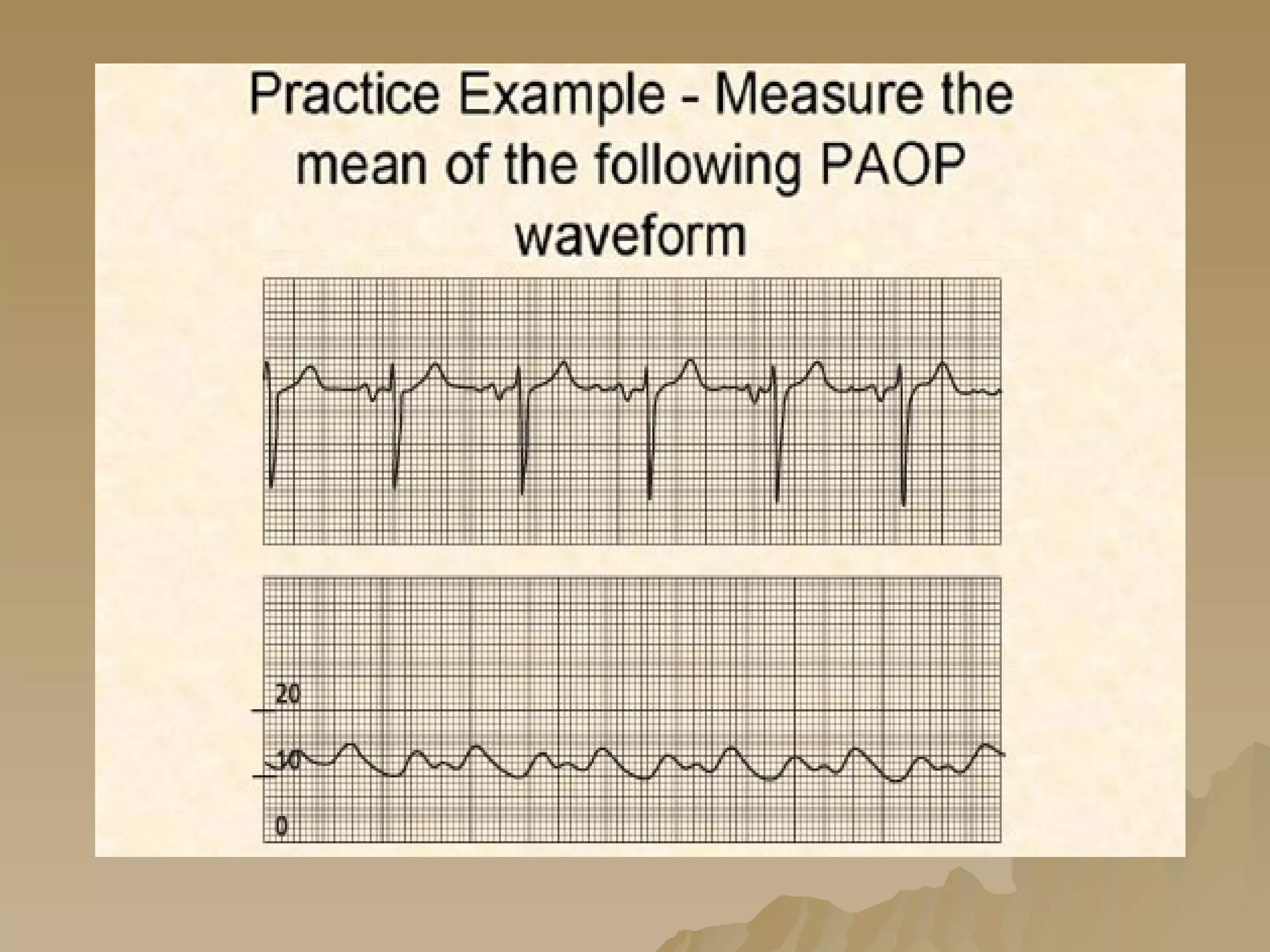
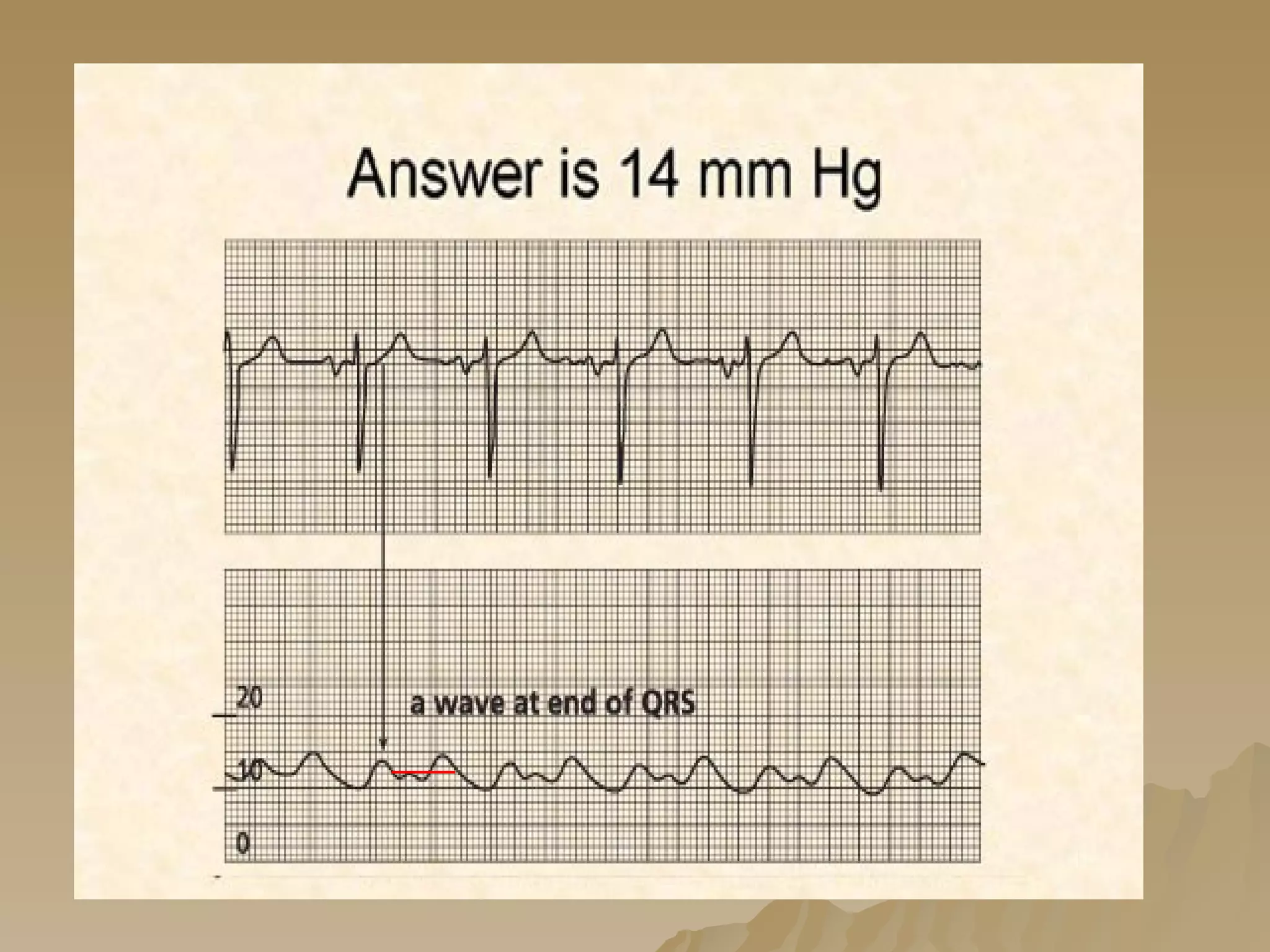
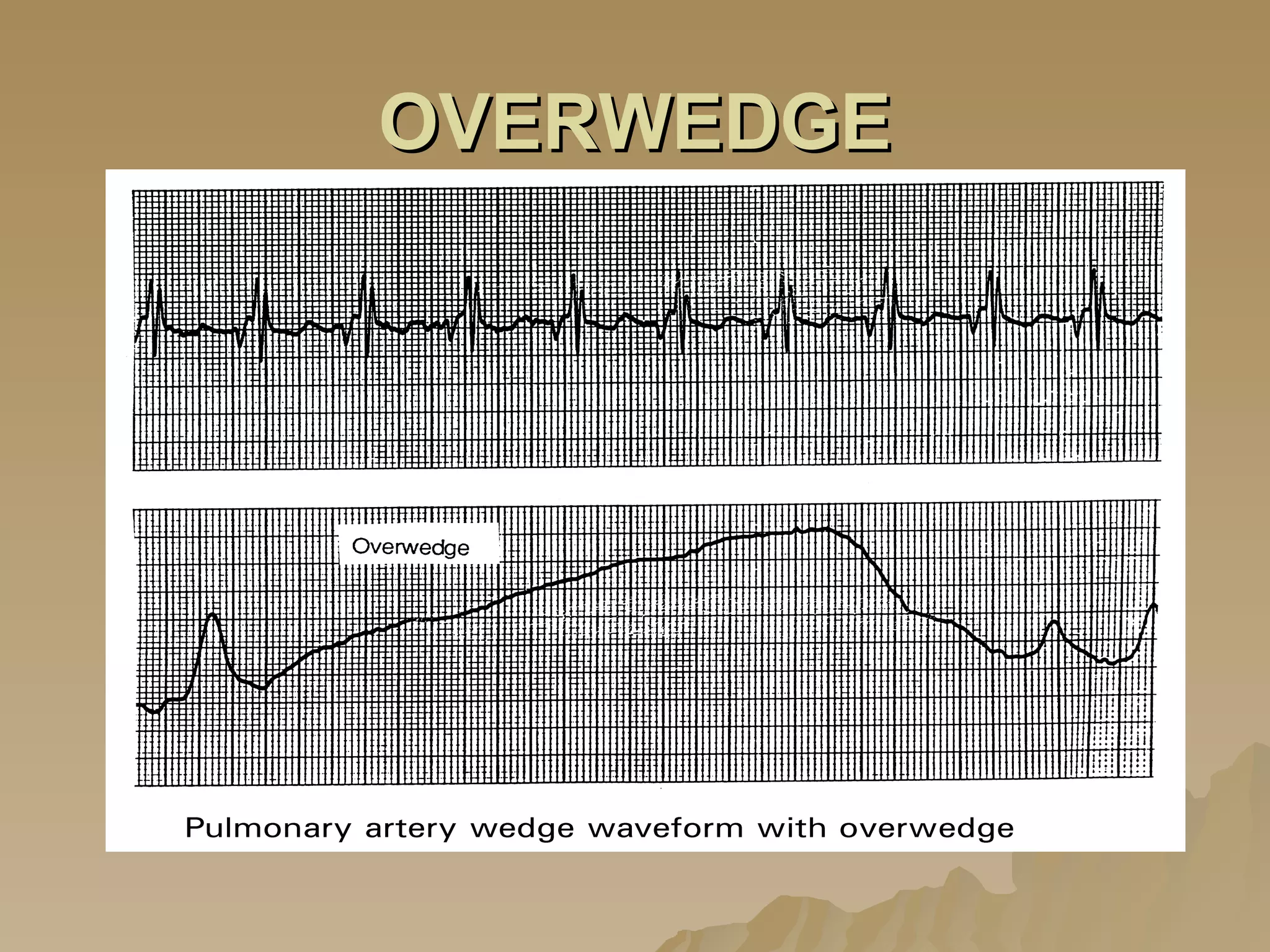
3. A pulmonary artery catheter allows for continuous monitoring of pressures, flows, oxygen saturation and calculation of cardiac output, and helps precisely manage fluid balance and hemodynamics.