1) Intra-aortic balloon counterpulsation (IABP) provides systolic unloading and diastolic augmentation to improve cardiac output.
2) IABP is indicated for cardiogenic shock, high-risk PCI/CABG, and mechanical complications.
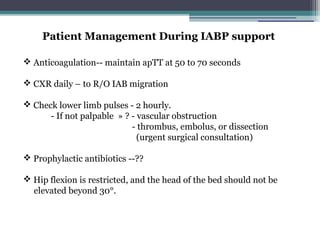
3) Potential complications include limb ischemia, infection, bleeding, and aortic injury.
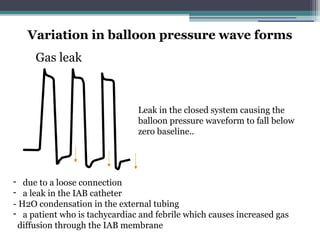
4) Optimal IABP waveform analysis and timing are important to maximize hemodynamic support.