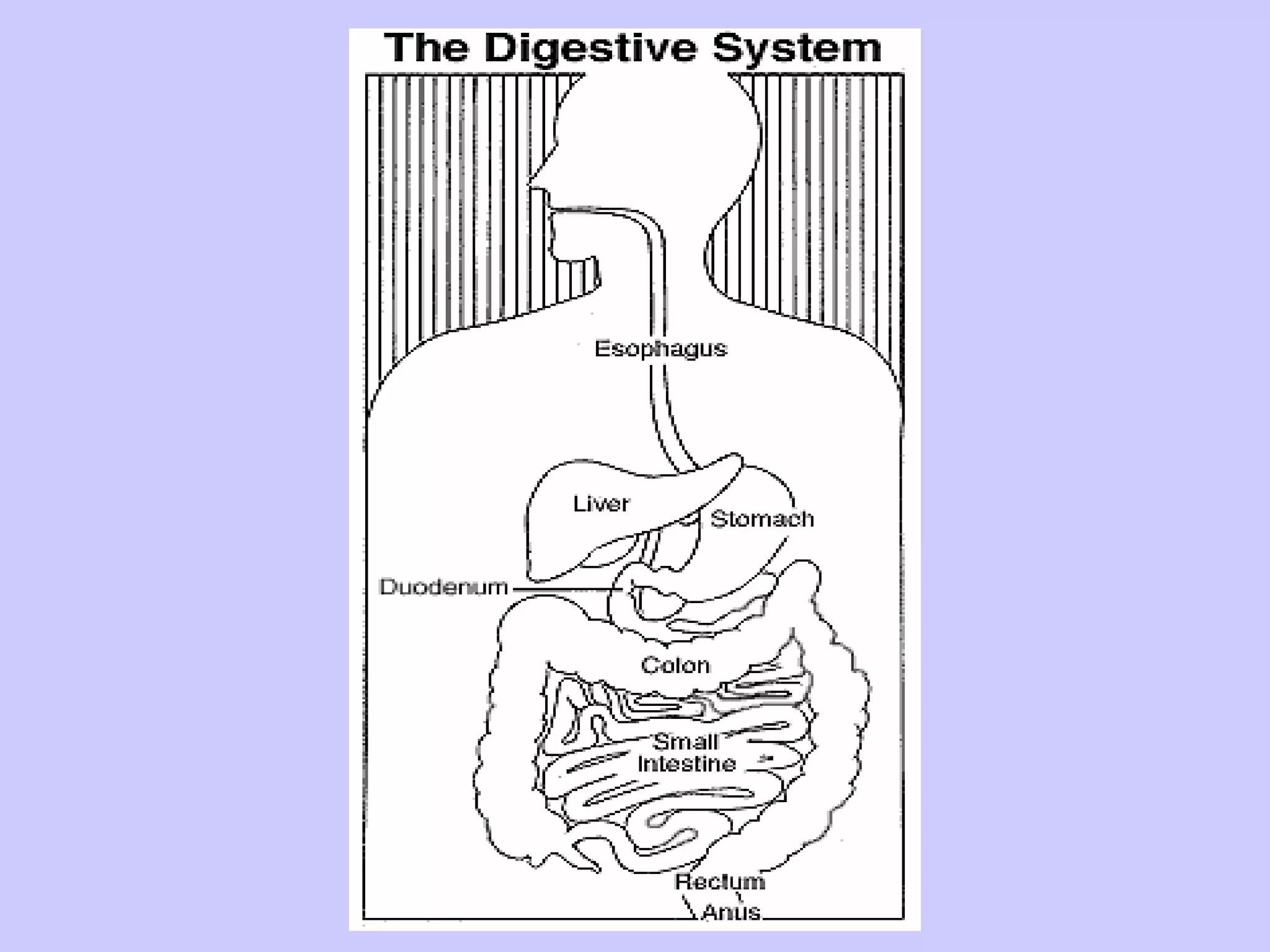
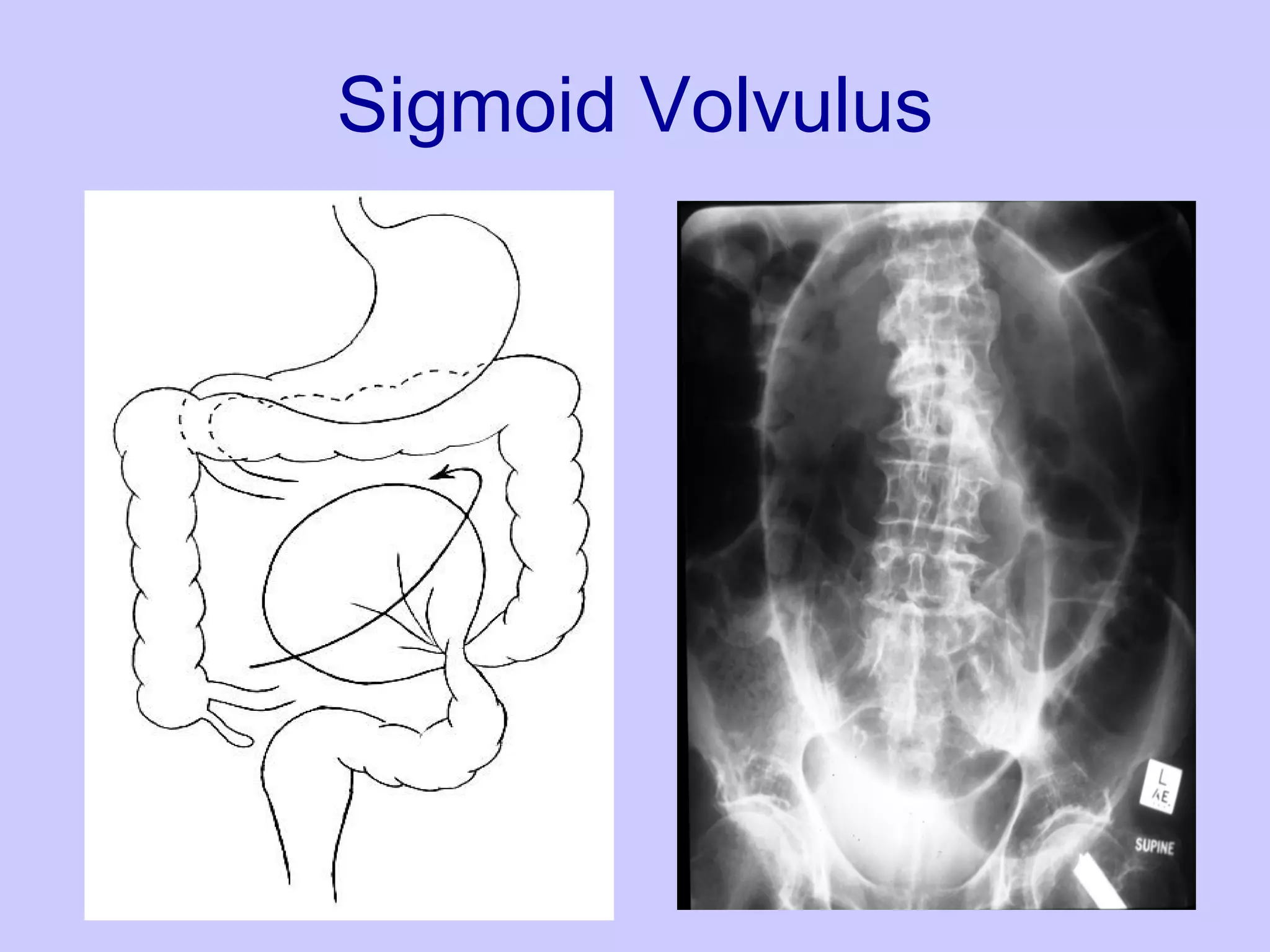
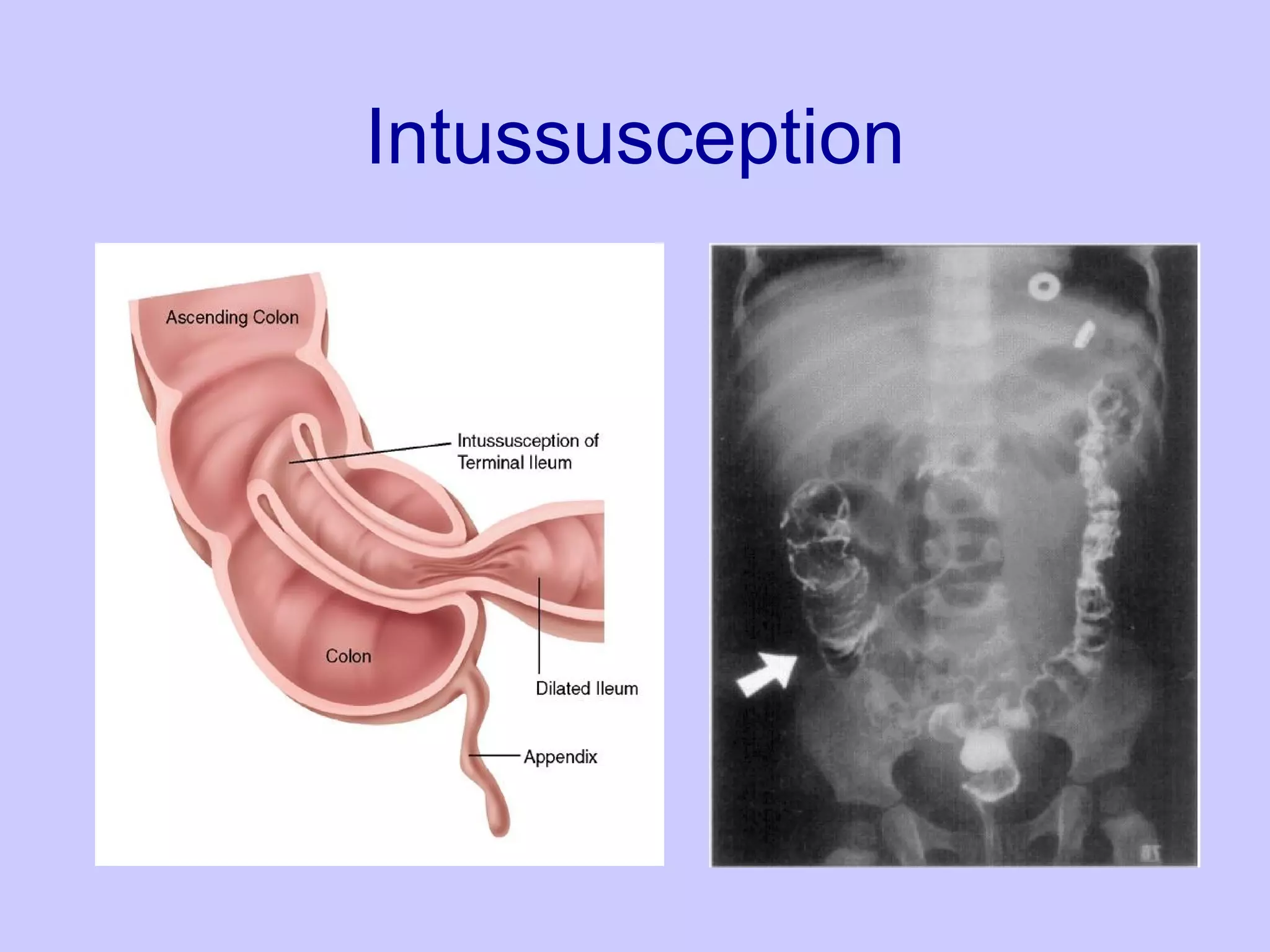
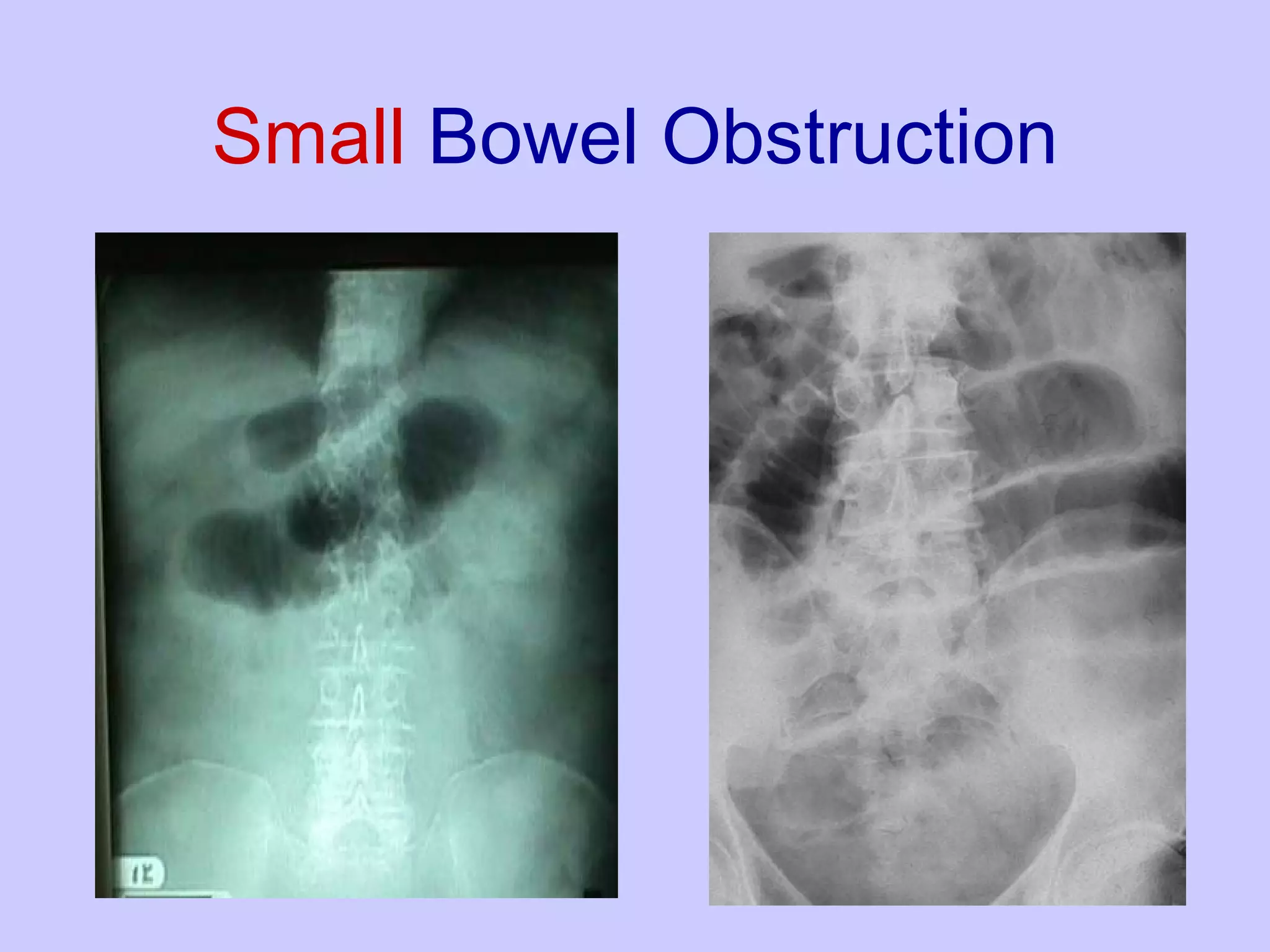
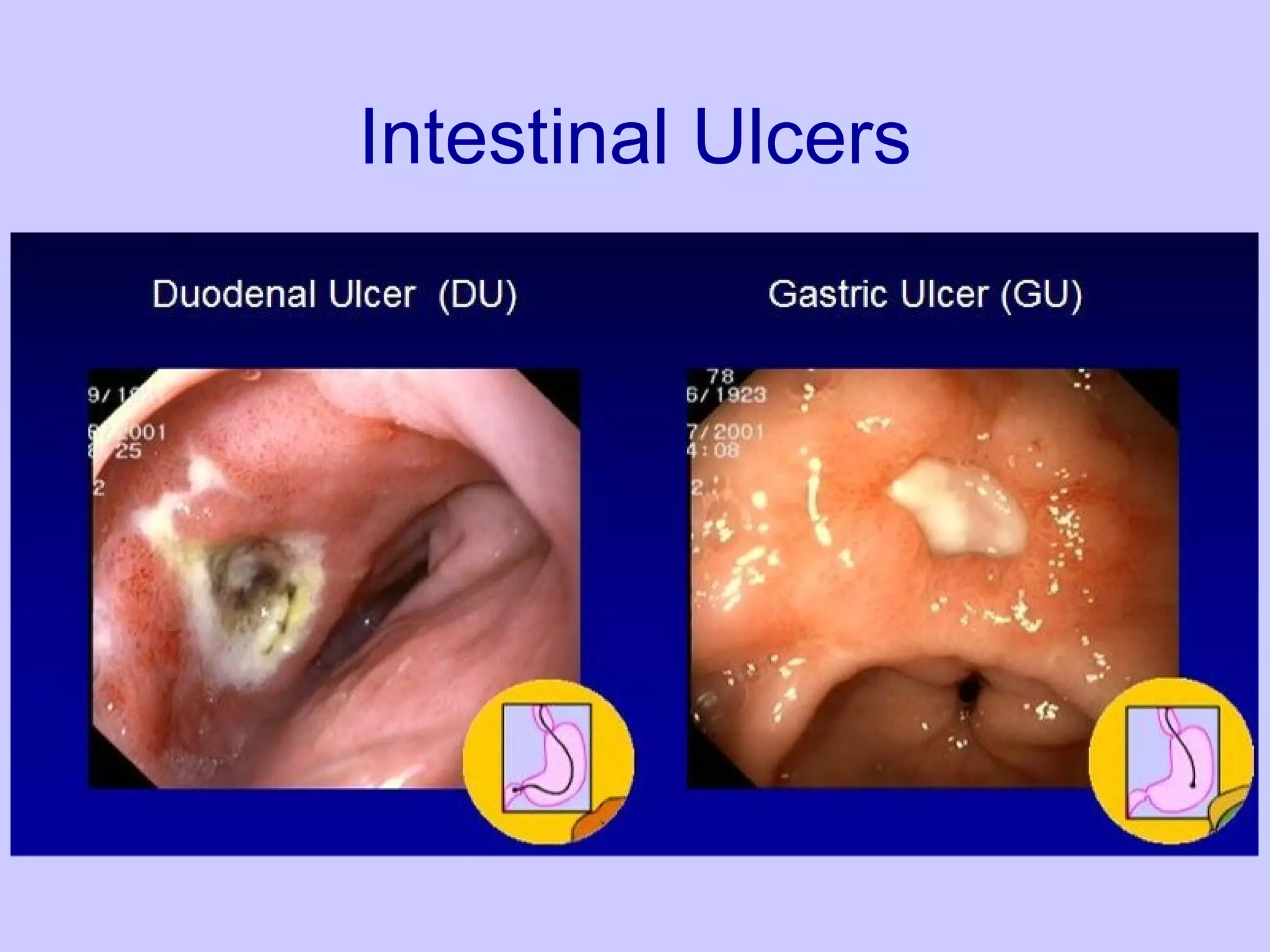
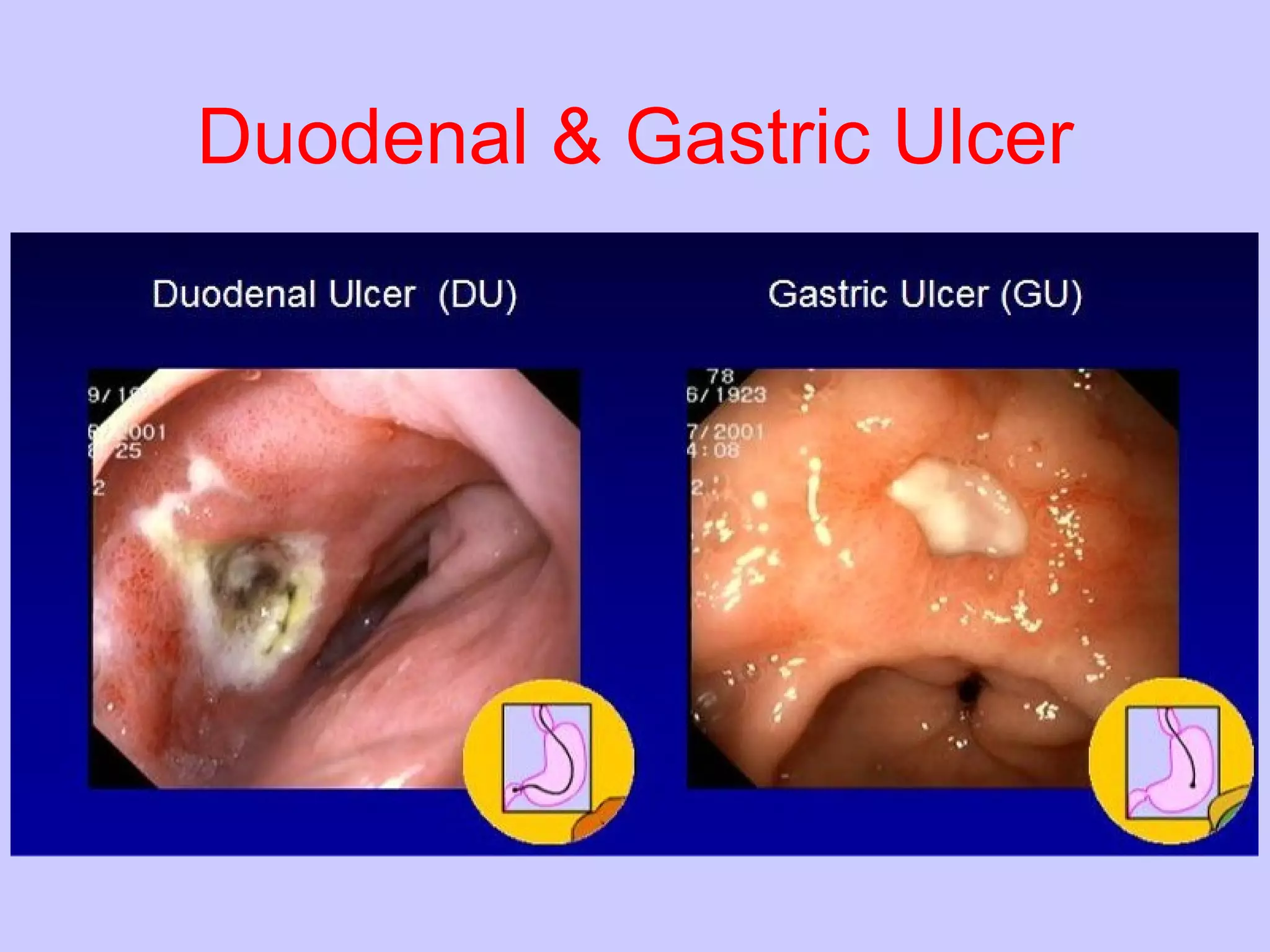
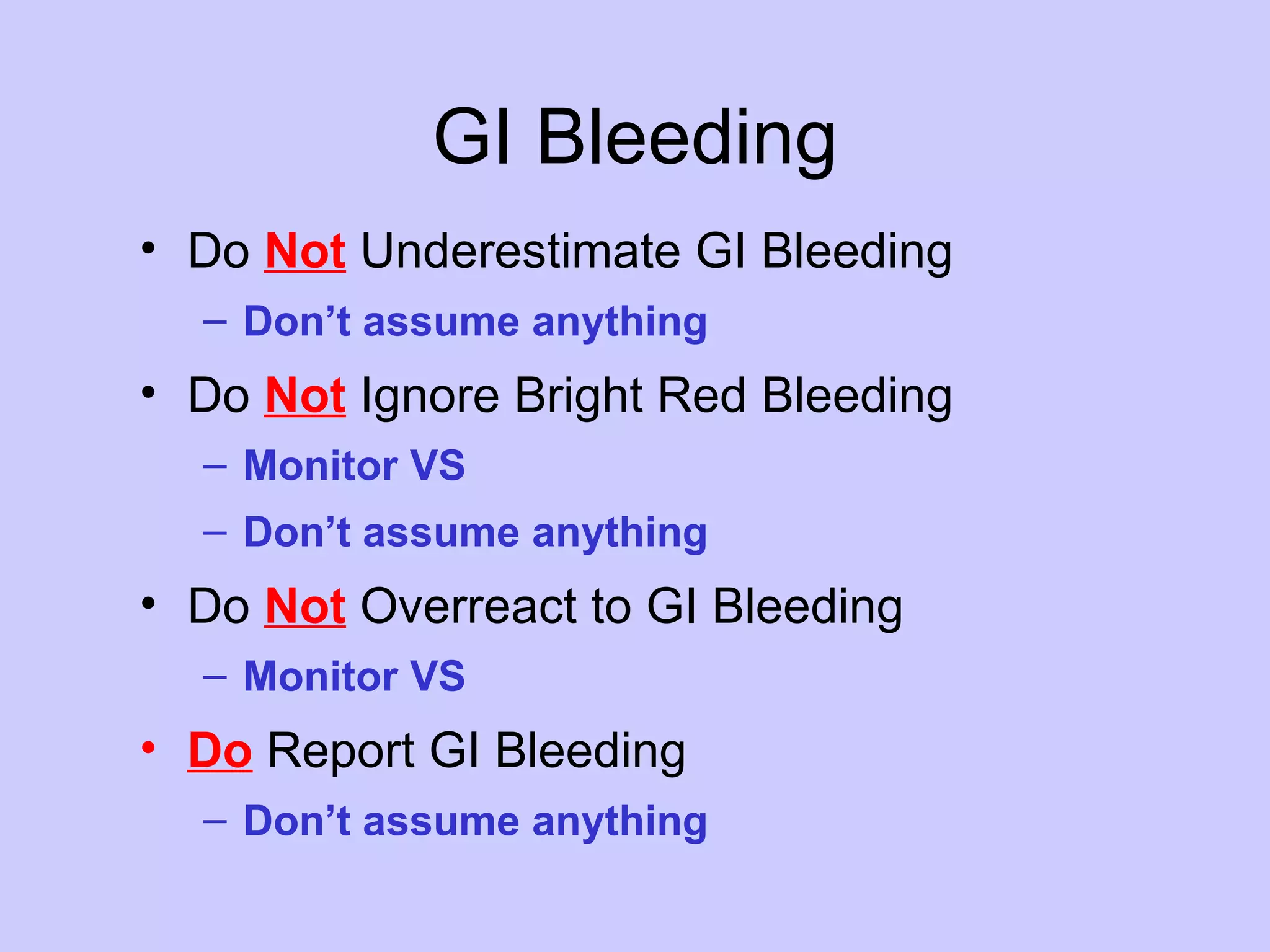
The document discusses various gastrointestinal disorders including intestinal obstructions, peptic ulcer disease, bowel disorders like ulcerative colitis and Crohn's disease, gastric cancer, colorectal cancer, and terms related to gastrointestinal bleeding. It provides details on causes, signs and symptoms, risk factors, treatments, and methods to localize sources of bleeding for different gastrointestinal conditions.



![References Fundamentals of Diagnostic Radiology, 2nd edition (1999). Brant, William E. & Helms, Clyde A., eds. Williams and Wilkins, Baltimore MD. Delabrousse, E., Destrumelle N., Brunelle S., Clair C., Mantion G., Kastler B. (2003) CT of small bowel obstruction in adults. Abdominal Imaging 28(2): 257-266. www.uptodate.com: Clinical manifestations and diagnosis of small bowel obstruction; Treatment of small bowel obstruction; Abdominal wall and groin hernias. Hansen, M. (1998). Pathophysiology: Foundations of disease and clinical intervention. Philadelphia: Saunders. http://www.medscape.com Givens BA, Simmons SJ: Gastroenterology in Clinical Nursing. 4th ed. St. Louis, Mo: C.V. Mosby Co, 1984. Ripamonti C, Bruera E: Palliative management of malignant bowel obstruction. Int J Gynecol Cancer 12 (2): 135-43, 2002 Mar-Apr. [PUBMED Abstract] Potluri V, Zhukovsky DS: Recent advances in malignant bowel obstruction: an interface of old and new. Curr Pain Headache Rep 7 (4): 270-8, 2003. [PUBMED Abstract] Baron TH: Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 344 (22): 1681-7, 2001. PUBMED Abstract] Mercadante S: Assessment and management of mechanical bowel obstruction. In: Portenoy RK, Bruera E, eds.: Topics in Palliative Care. Volume 1. New York, NY: Oxford University Press, 1997, pp. 113-30.](https://image.slidesharecdn.com/gastrointestinaldisorders-090529203508-phpapp02/75/Gastrointestinal-Disorders-61-2048.jpg)
![References Givens BA, Simmons SJ: Gastroenterology in Clinical Nursing. 4th ed. St. Louis, Mo: C.V. Mosby Co, 1984. Ripamonti C, Bruera E: Palliative management of malignant bowel obstruction. Int J Gynecol Cancer 12 (2): 135-43, 2002 Mar-Apr. [PUBMED Abstract] Potluri V, Zhukovsky DS: Recent advances in malignant bowel obstruction: an interface of old and new. Curr Pain Headache Rep 7 (4): 270-8, 2003. [PUBMED Abstract] Baron TH: Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 344 (22): 1681-7, 2001. PUBMED Abstract] Mercadante S: Assessment and management of mechanical bowel obstruction. In: Portenoy RK, Bruera E, eds.: Topics in Palliative Care. Volume 1. New York, NY: Oxford University Press, 1997, pp. 113-30.](https://image.slidesharecdn.com/gastrointestinaldisorders-090529203508-phpapp02/75/Gastrointestinal-Disorders-62-2048.jpg)