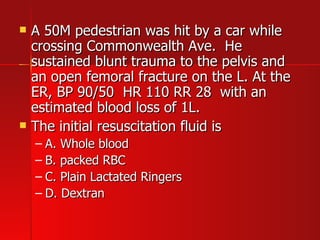
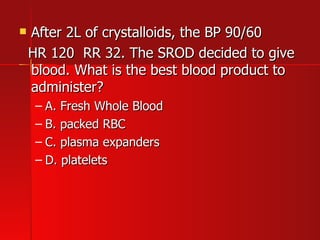
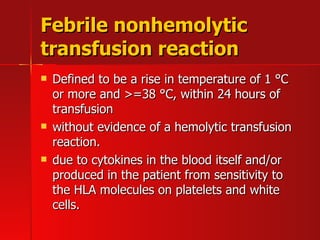
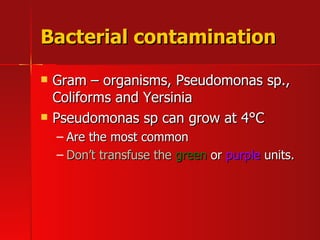
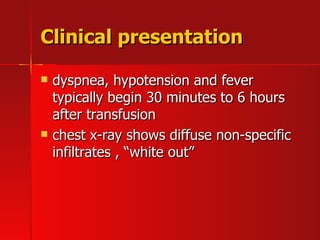
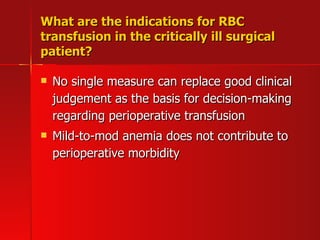
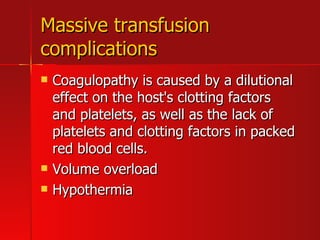
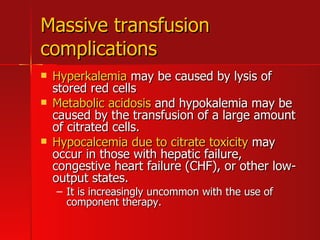
The document discusses various functions and properties of blood, including transport, regulation, and protection. It then summarizes different blood products like packed red blood cells, platelets, fresh frozen plasma, and cryoprecipitated antihemophilic factor. It discusses their indications, storage requirements, and risks of transfusion such as allergic reactions, hemolytic reactions, febrile reactions, bacterial contamination, transfusion-related acute lung injury, and disease transmission.