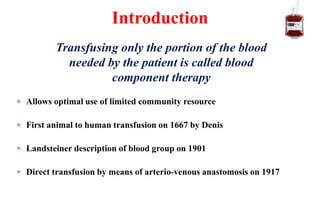
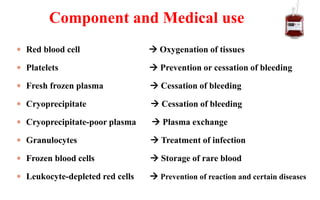
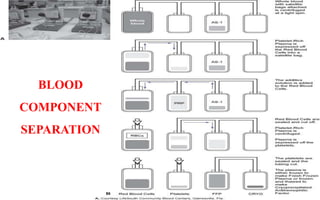
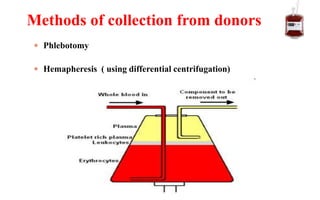
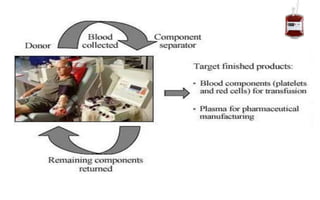
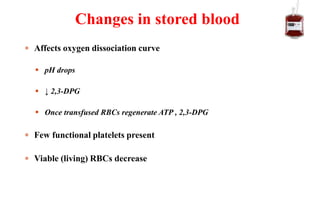
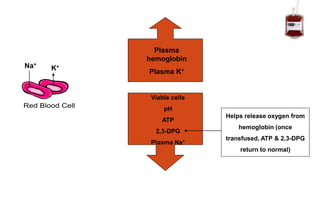
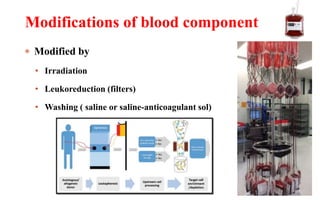
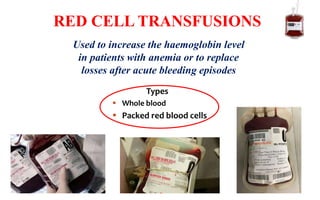
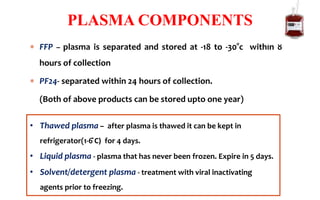
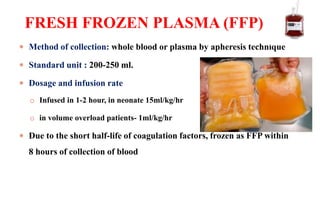
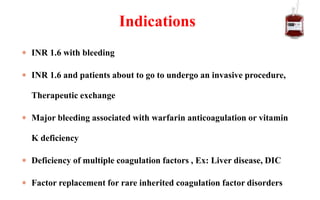
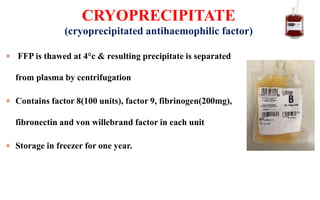
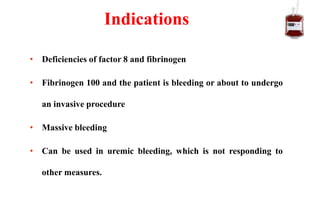
Blood component therapy involves transfusing only the necessary components of blood needed by a patient. This reduces waste and risks compared to whole blood transfusions. The main components are red blood cells, platelets, fresh frozen plasma, and cryoprecipitate. Each component has specific functions and indications for use in treating conditions like anemia, bleeding, or coagulation disorders. Proper collection, storage, and modification of the components helps maintain their viability and functions.

![[To treat active bleeding]
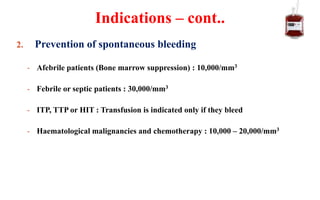
Count must be kept above 50,000/mm3 in most bleeding situations
In DIC and central nervous system bleeding , cut off is 1,00,000/mm3
Bleeding on anti platelet medication
Indications
(Therapeutic)](https://image.slidesharecdn.com/bloodcomponentstherapy-191026203514/85/Blood-components-32-320.jpg)
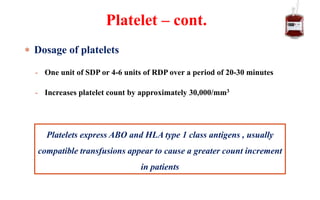
![1. Preparation for an invasive procedure :
• Neurosurgery or Ocular surgery : 1,00,000/mm3
• Major surgery : 50,000/mm3
• Endoscopic procedures : 50,000/mm3 for therapeutic
: 20,000/mm3 for diagnostic
• Central line placement : 20,000/mm3
• Lumbar puncture : 40,000/mm3 to 50,000/mm3
• Epidural anaesthesia : 80,000/mm3
• Bone marrow aspiration : 20,000/mm3
(Can be done with lower counts with applying pressure at site of procedure)
Indications
(Prophylactic)
[To prevent spontaneous bleeding]](https://image.slidesharecdn.com/bloodcomponentstherapy-191026203514/85/Blood-components-33-320.jpg)