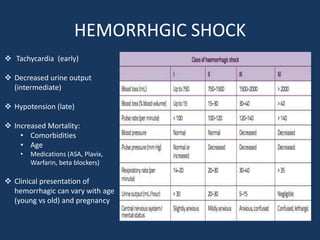
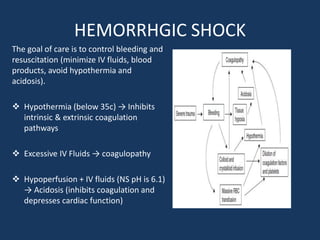
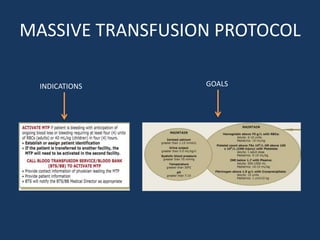
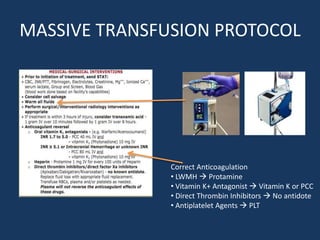
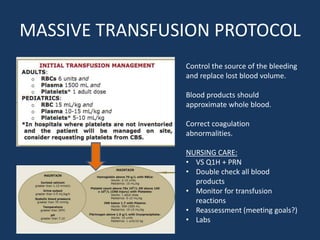
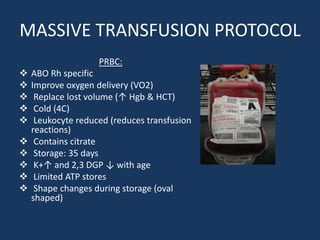
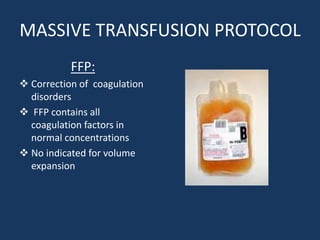
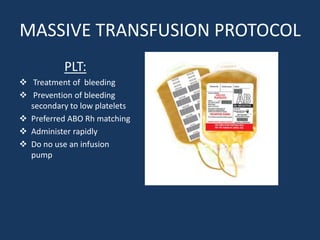
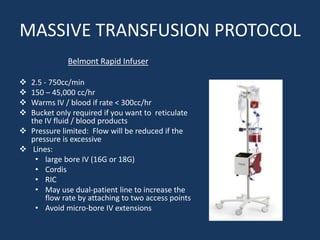
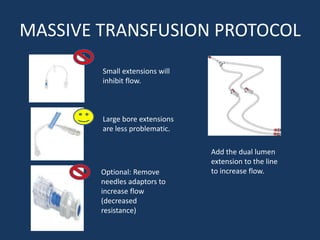
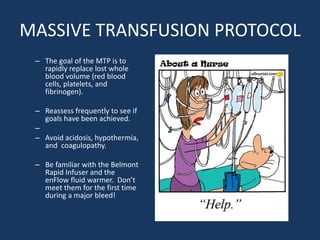
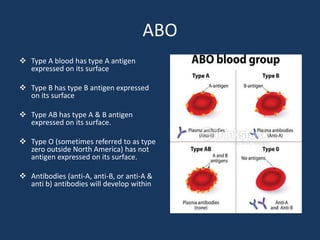
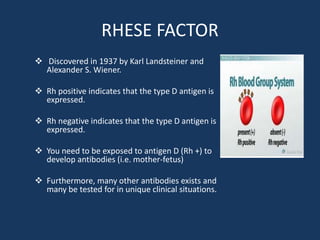
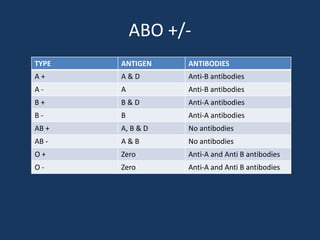
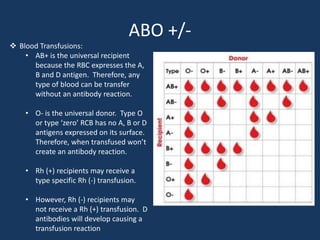
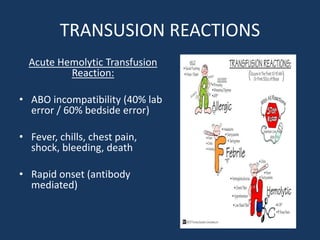
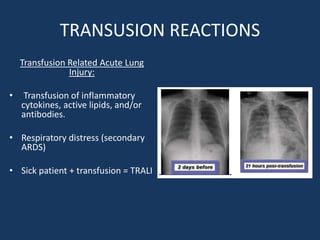
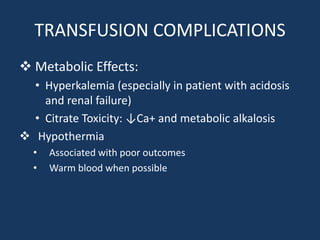
The document reviews massive transfusion protocols (MTPs) focusing on the management of hemorrhagic shock and the associated risks and complications. It outlines the goals of MTPs, which include aggressive coagulation factor therapy, minimizing crystalloid infusion, and preventing coagulopathy, hypothermia, and acidosis during treatment. Additionally, it discusses blood type compatibility for transfusions and potential adverse reactions, emphasizing the importance of monitoring and reassessment during massive transfusions.