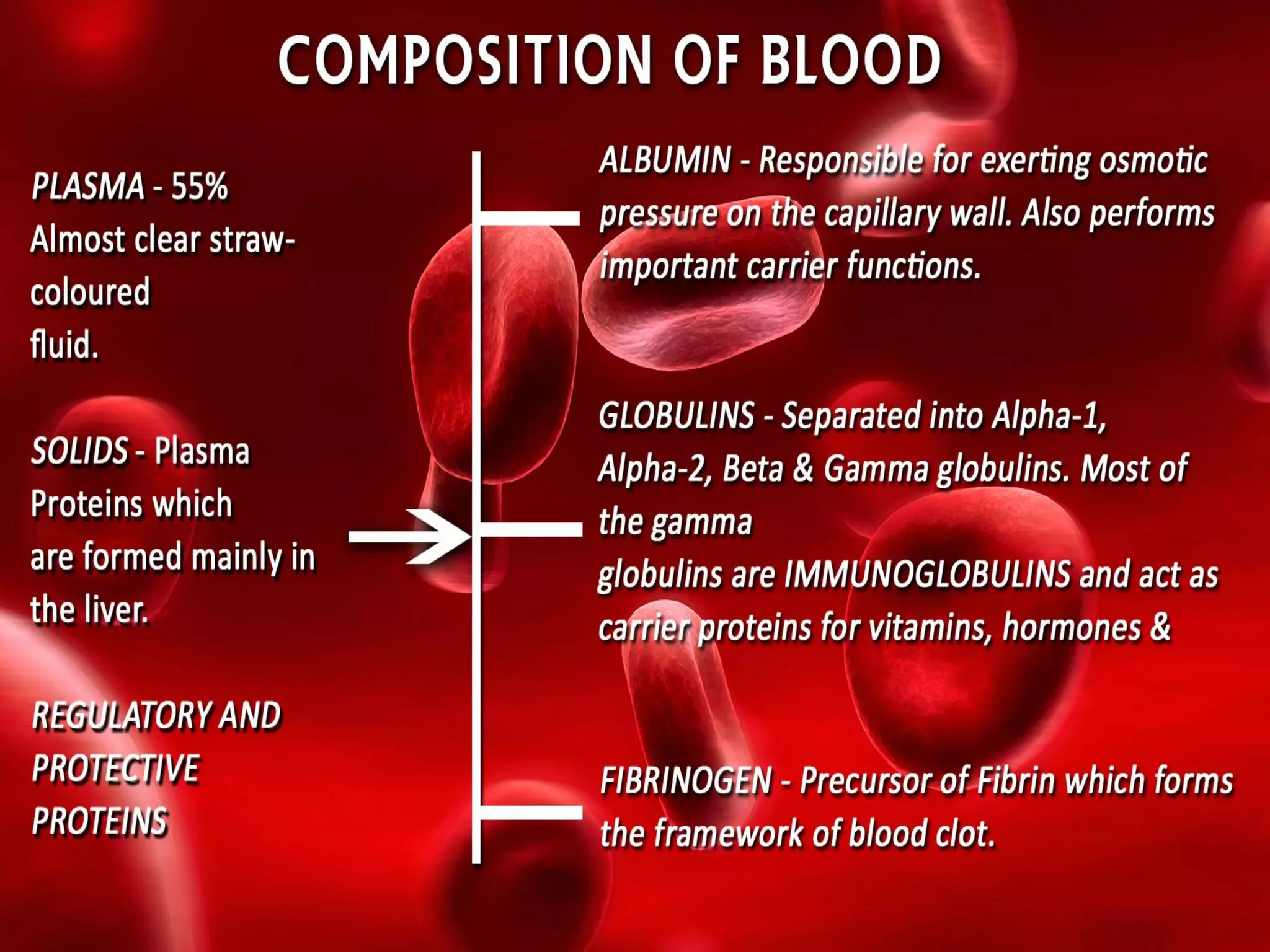
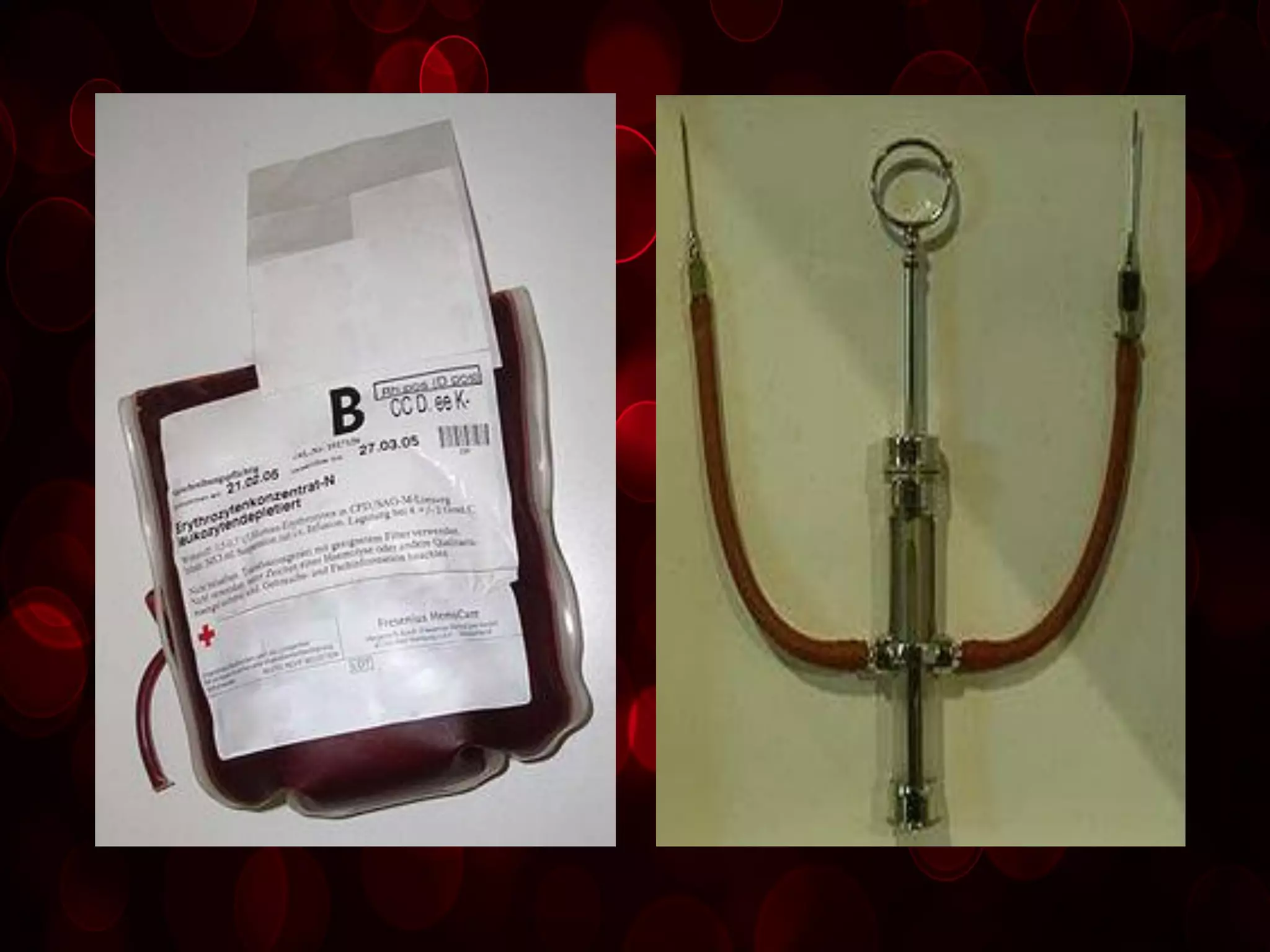
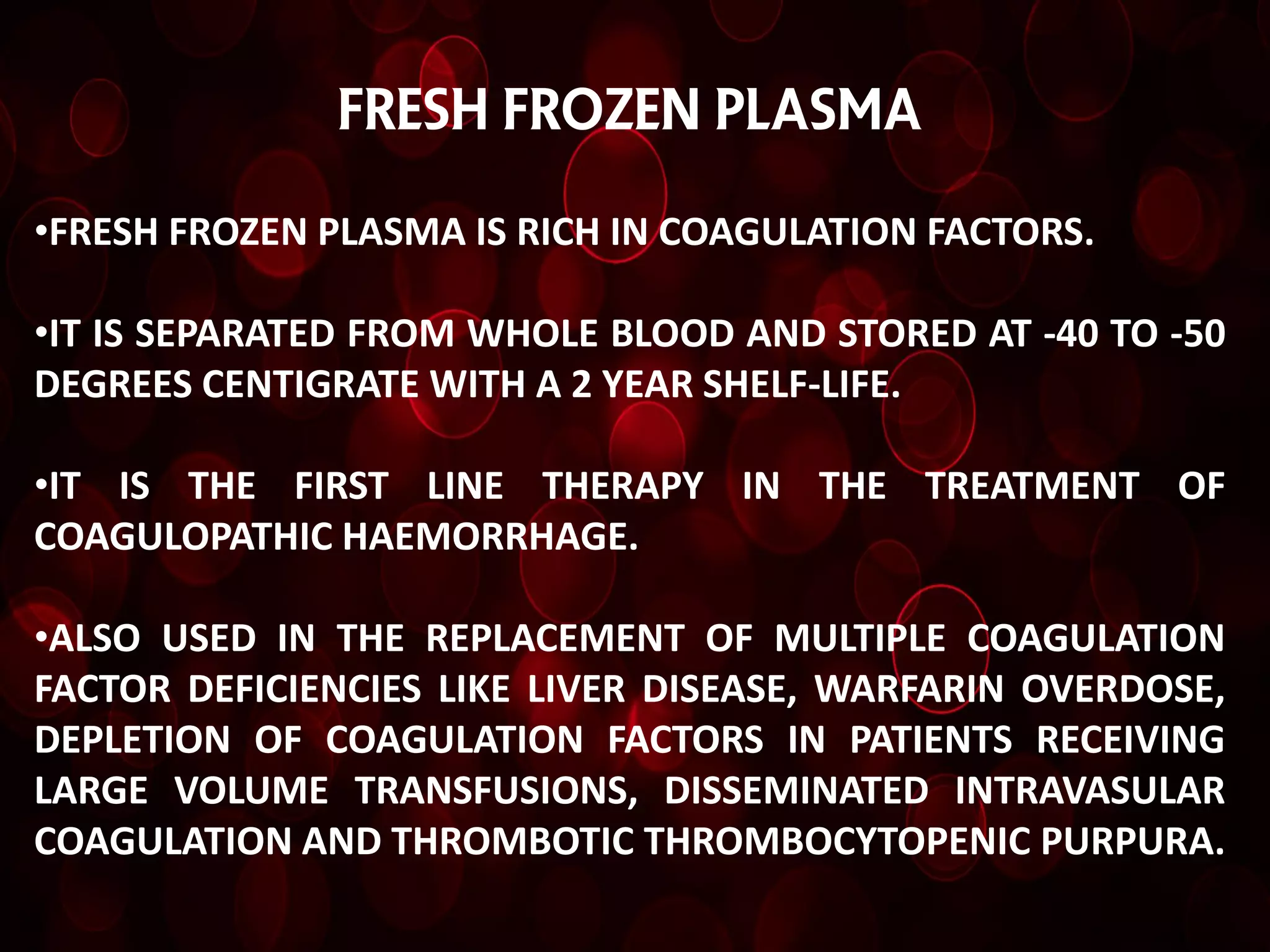
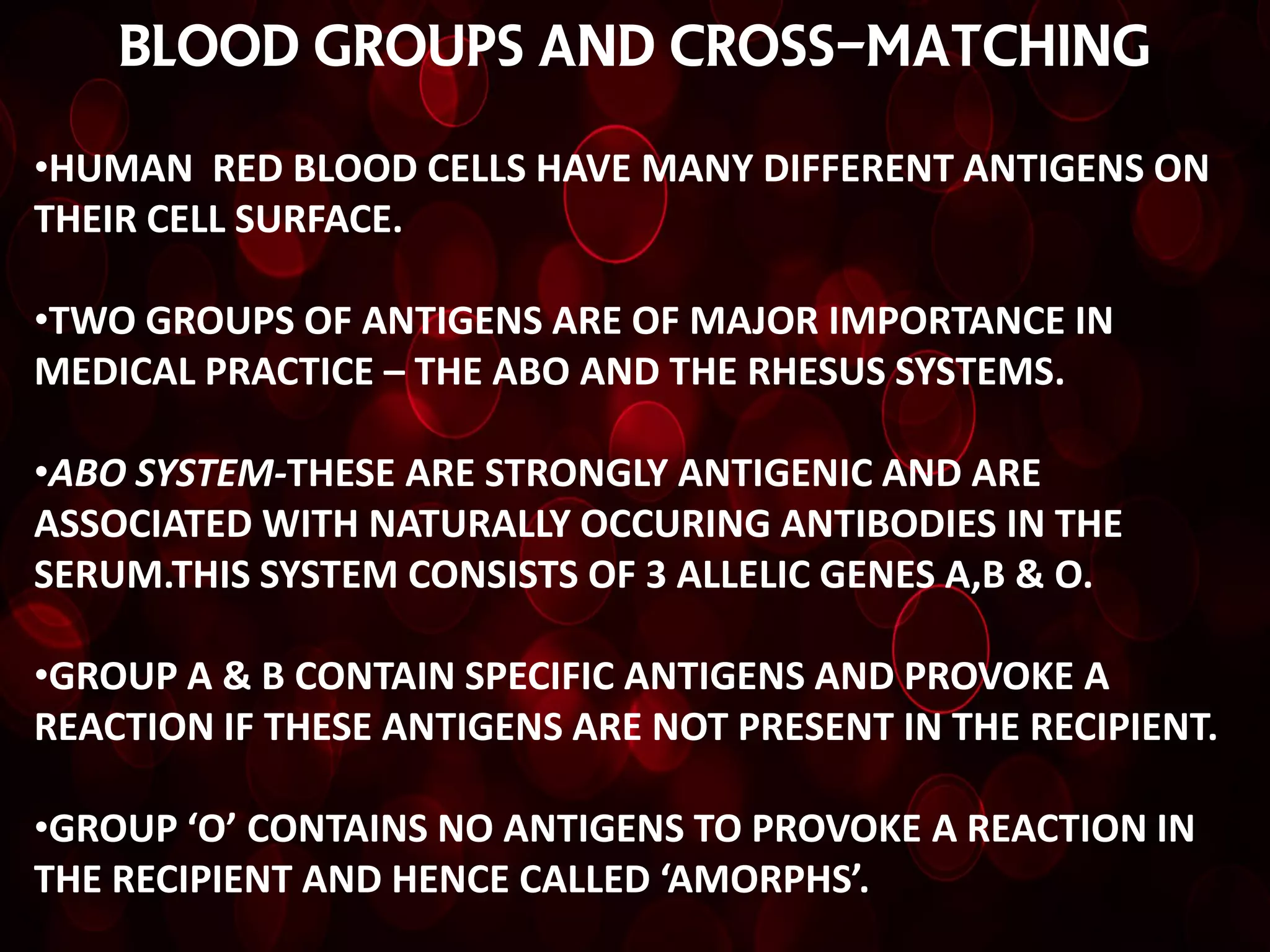
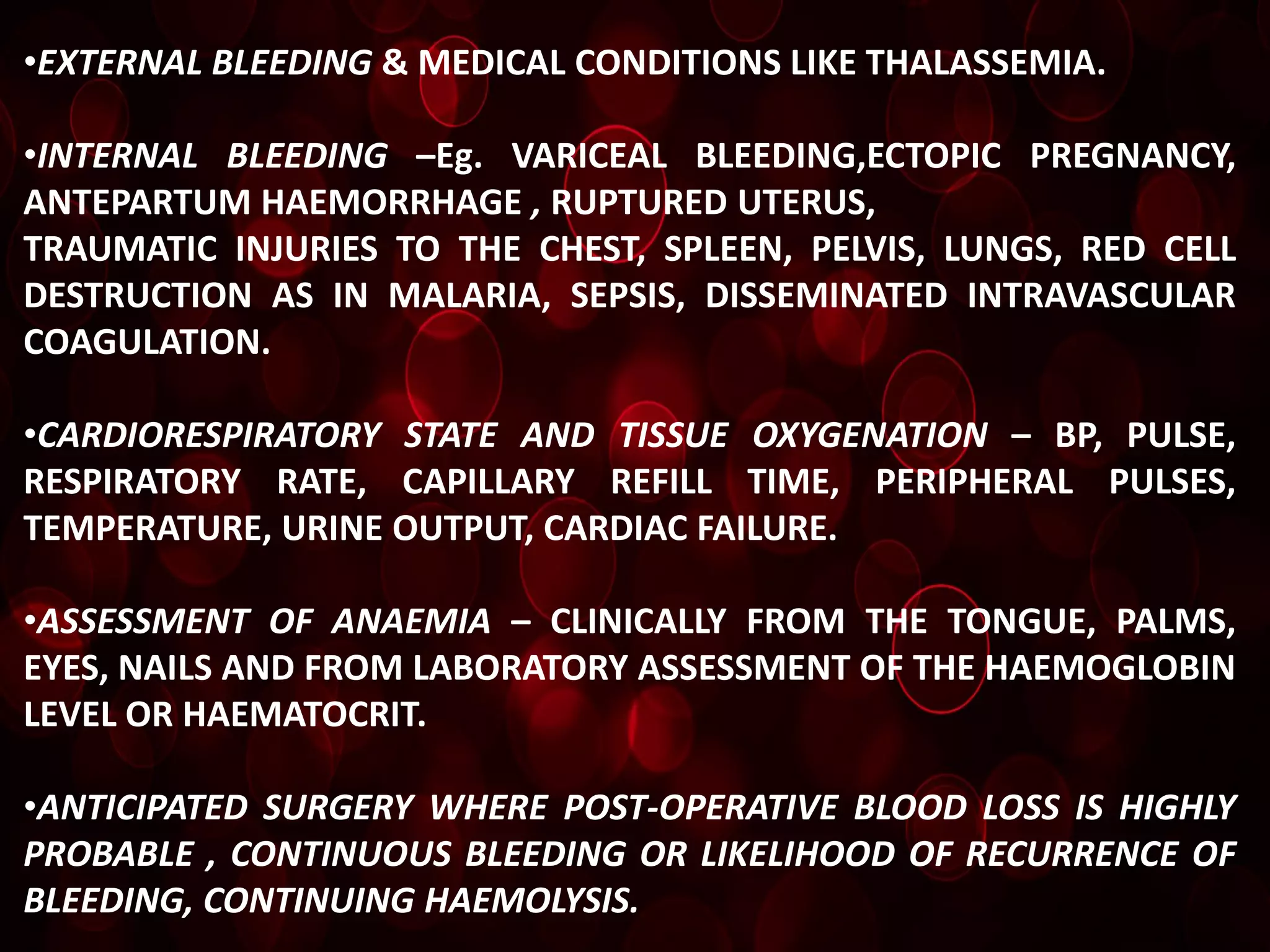
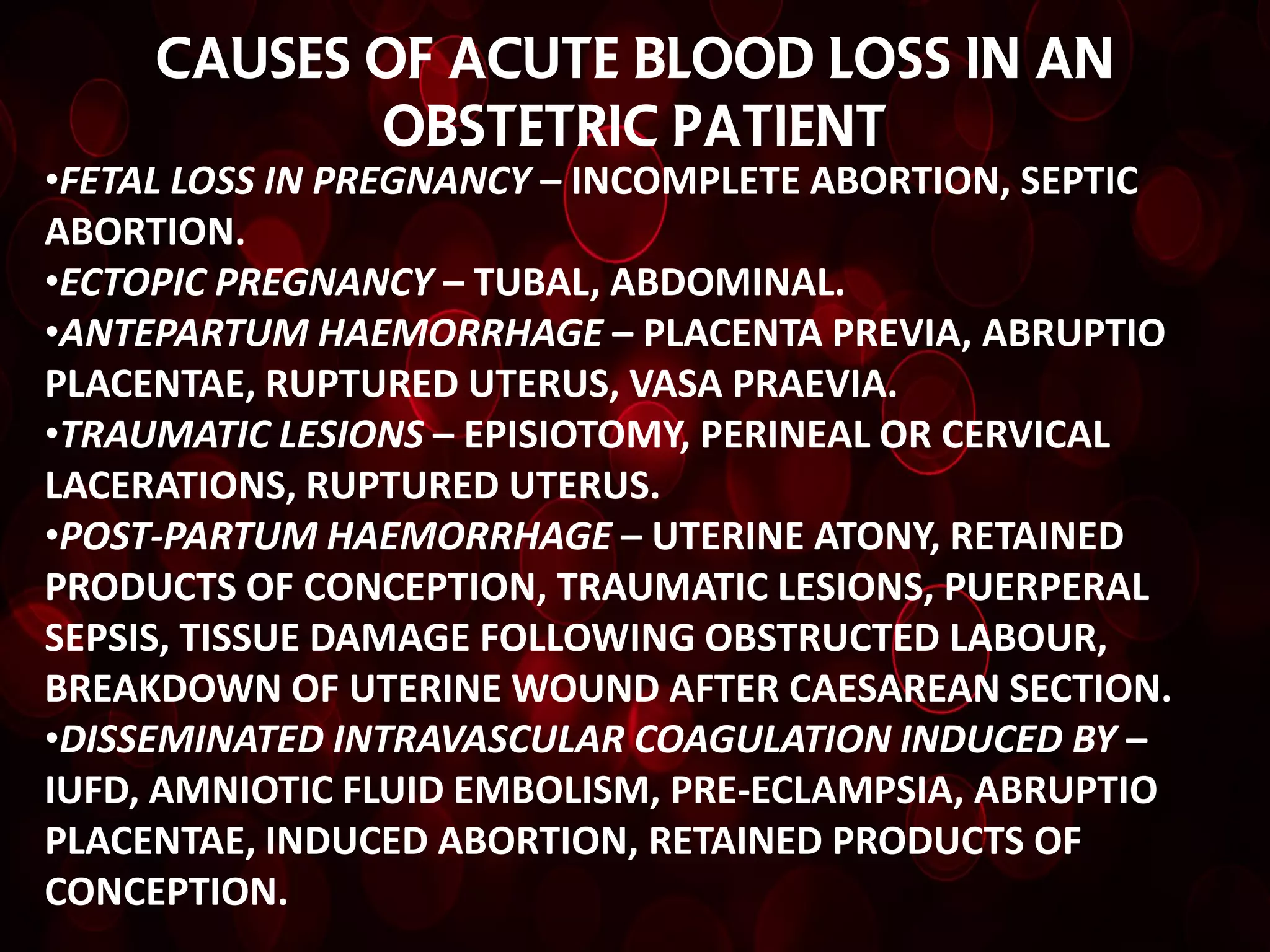
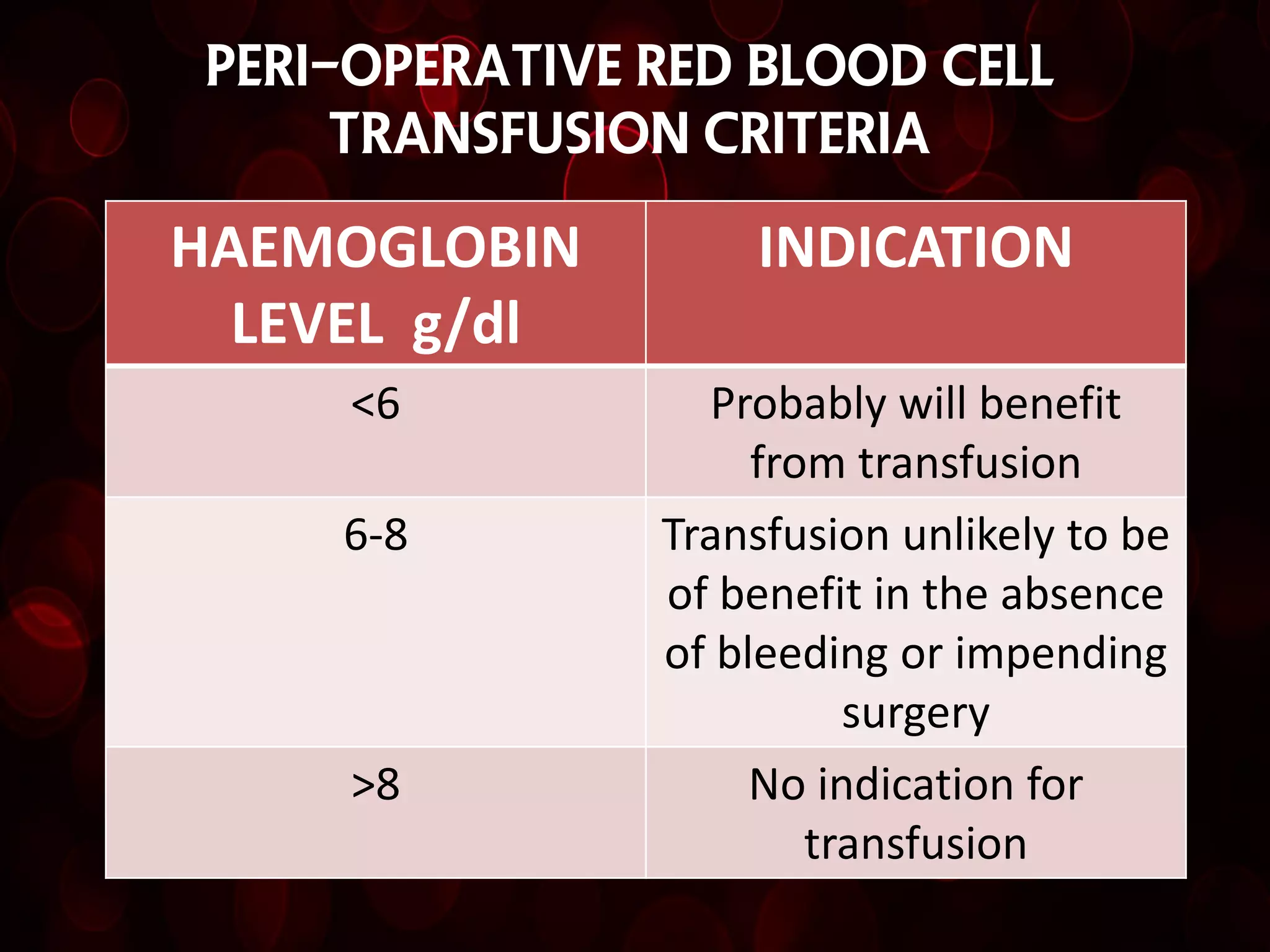
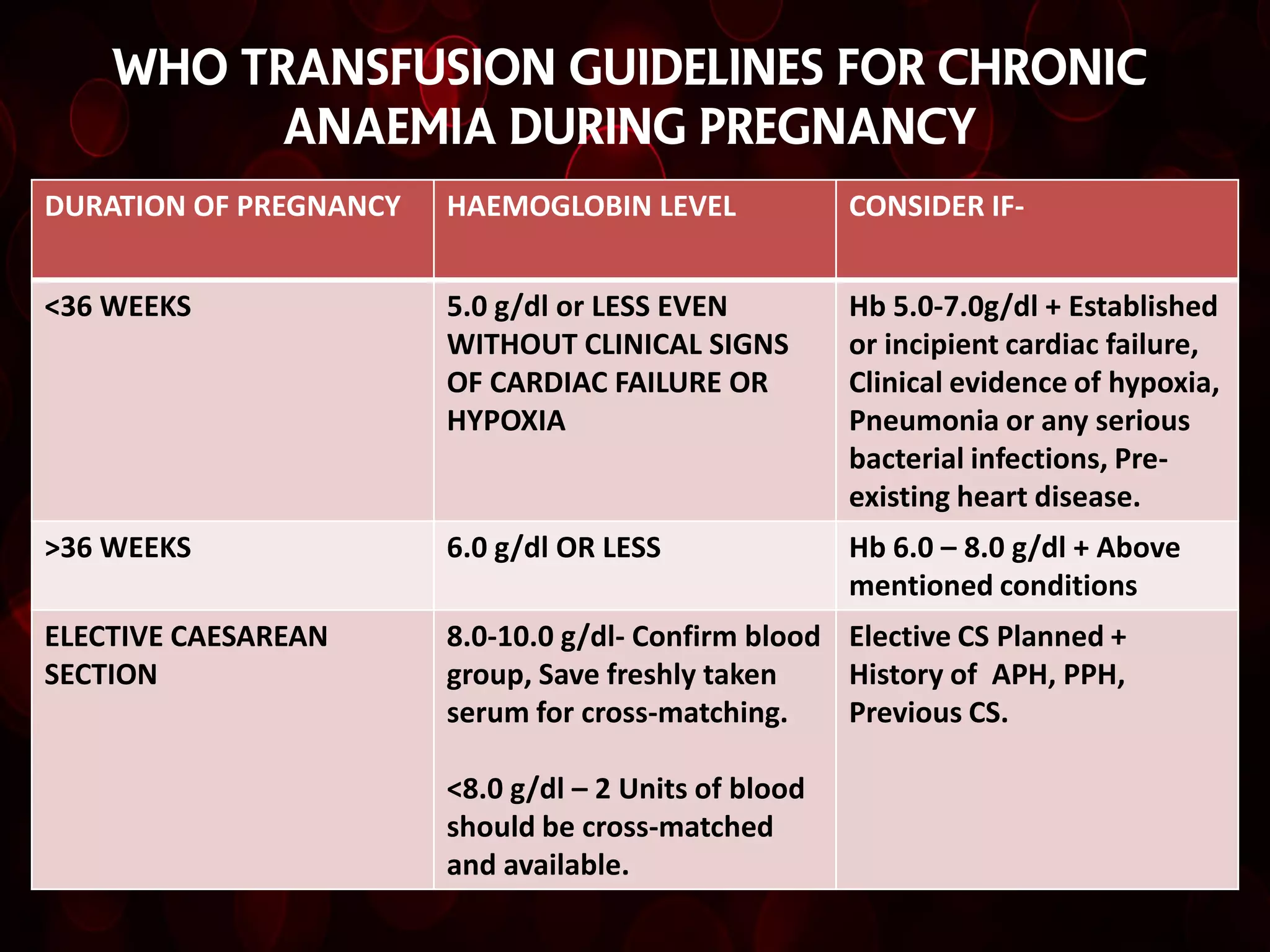
This document discusses blood transfusion, including definitions, types of transfusions, blood products, indications for transfusion, risks, and guidelines. It covers topics like whole blood, packed red blood cells, platelets, plasma, and cryoprecipitate. Key points include that transfusion involves receiving blood products intravenously to replace lost blood, it can use one's own blood or from a donor, and decisions should be based on careful assessment of clinical and lab indications to save life or prevent morbidity.