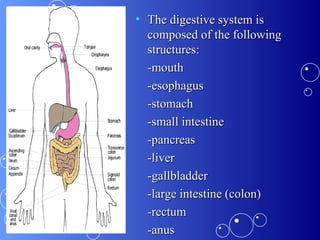
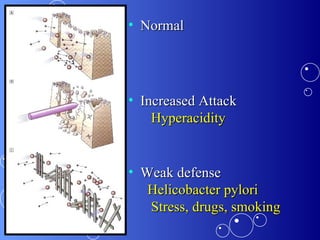
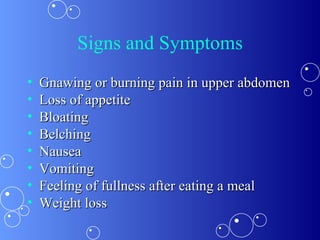
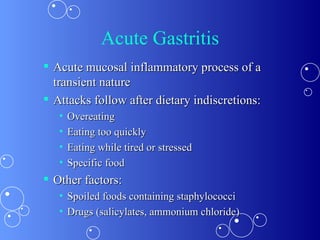
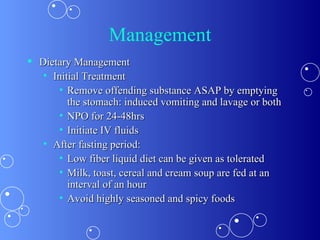
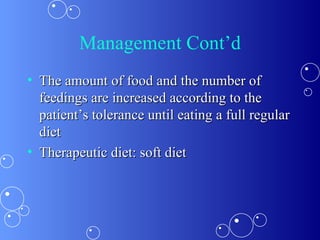
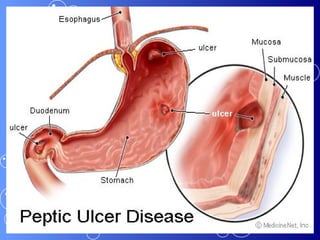
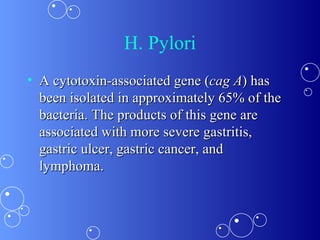
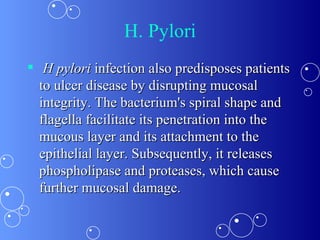
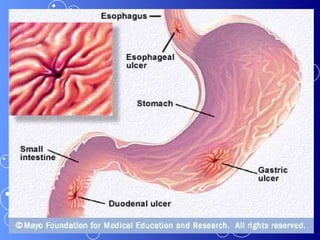
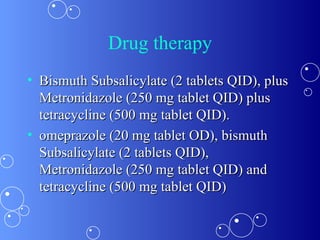
This document discusses the dietary management of various gastrointestinal diseases including diarrhea, constipation, gastritis, and peptic ulcers. It describes the anatomy and functions of the digestive system. It defines different types of constipation and diarrhea and their causes. Dietary recommendations are provided for different GI conditions, focusing on fluid and fiber intake, meal patterns, and avoiding irritating foods. Medical treatments including drugs and H. pylori eradication therapies are also summarized.




![References Soll AH. Consensus conference. Medical treatment of peptic ulcer disease. Practice guidelines. Practice Parameters Committee of the American College of Gastroenterology. JAMA . Feb 28 1996;275(8):622-9. [Medline] . Vaira D, Gatta L, Ricci C, et al. Peptic ulcer and Helicobacter pylori: update on testing and treatment. Postgrad Med . Jun 2005;117(6):17-22, 46. [Medline]](https://image.slidesharecdn.com/gitdiseasespresentnno-2appliednutrition-101002000551-phpapp01/85/Git-diseases-presentn-no-2-applied-nutrition-65-320.jpg)
