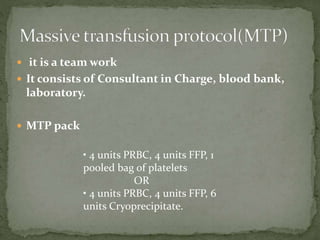
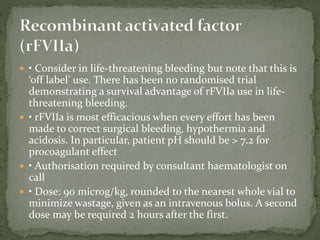
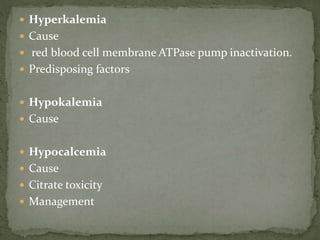
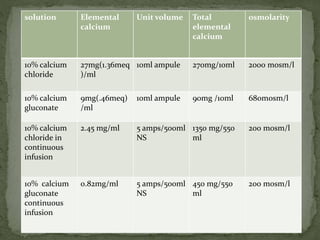
The document provides guidelines for managing massive blood transfusion or massive blood loss, defining it as replacing over 50% of total blood volume within 3 hours or 100% within 24 hours. It outlines the components of a massive transfusion protocol including blood products to transfuse and common complications to monitor for such as hypothermia, dilutional coagulopathy, and acidosis. The protocol is a multidisciplinary approach involving consultants, the blood bank, and laboratory to rapidly replace lost blood and clotting factors.