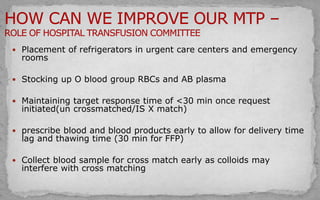
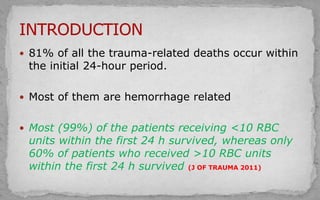
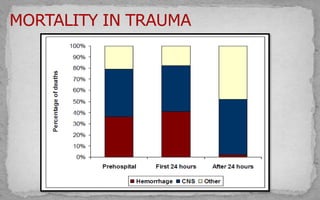
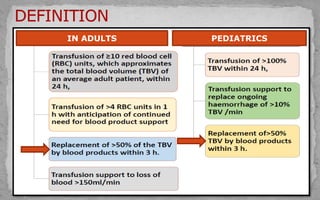
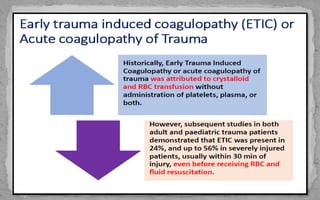
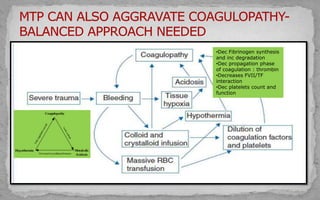
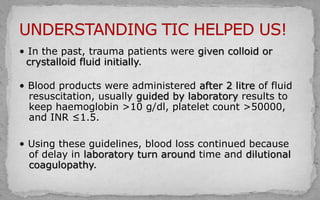
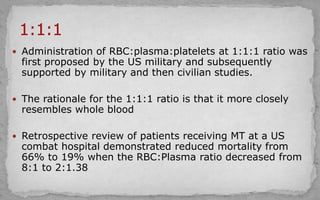
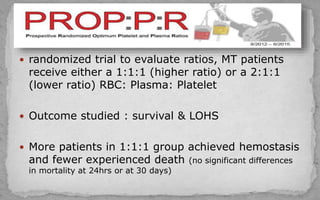
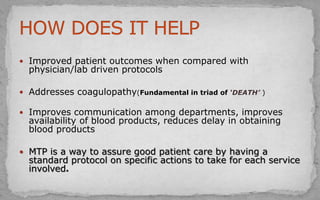
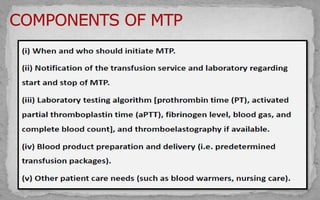
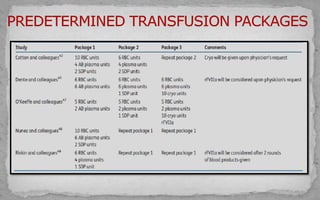
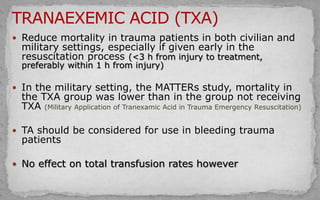
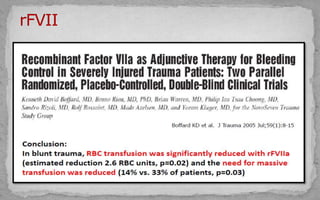
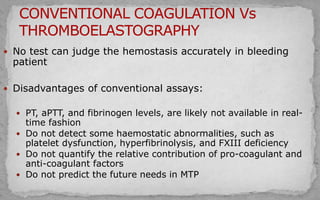
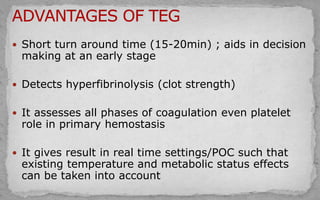
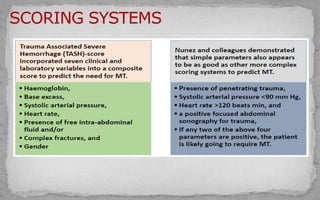
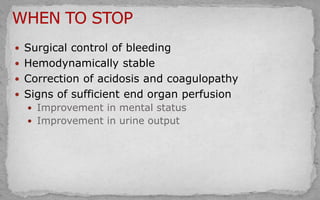
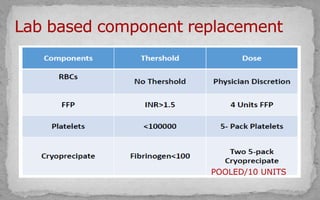
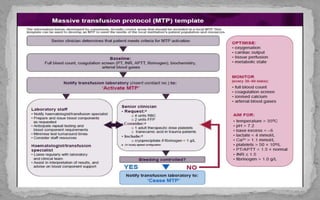
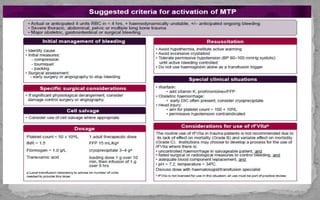
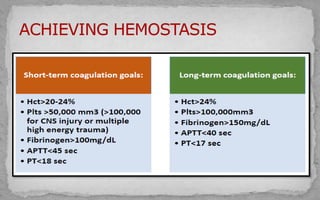
The document discusses trauma-related deaths and the importance of timely blood transfusions in stabilizing patients, focusing on a shift from traditional transfusion practices to more effective protocols like the 1:1:1 ratio of RBCs, plasma, and platelets to address coagulopathy and improve patient outcomes. It highlights the significance of early identification of patients at risk and the use of blood products in resuscitation to reduce mortality, particularly in military settings. Additionally, it emphasizes the need for standardized protocols to enhance communication, expedite blood product availability, and ensure better overall management of trauma patients.



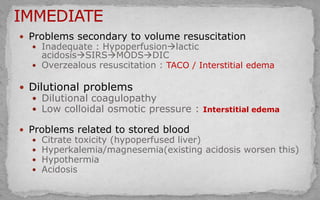
![ Significant role
Coagulation
Platelet adhesion
Cardiac and smooth muscle contractility
In the setting of hemorrhagic shock
Rapid infusion of blood products + decreased hepatic
clearance of citrate (hypoperfusion/hypothermia)
Causes hypocalcemia
A threshold ionized calcium [iCa] <0.9 mmol/L proposed as a
trigger for intravenous calcium](https://image.slidesharecdn.com/massivetransfusionprotocol-191015113244/85/Massive-transfusion-protocol-45-320.jpg)