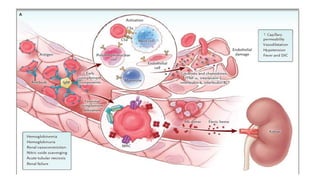
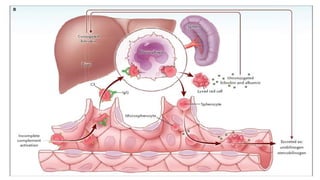
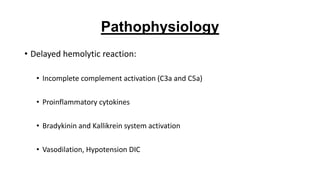
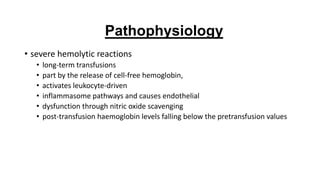
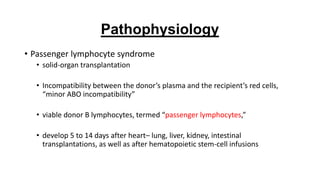
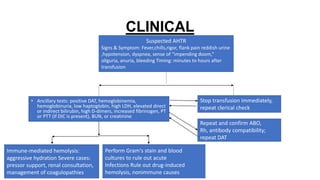
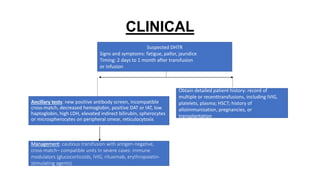
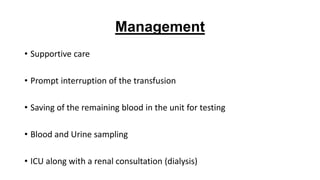
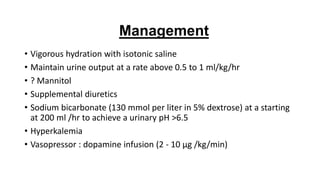
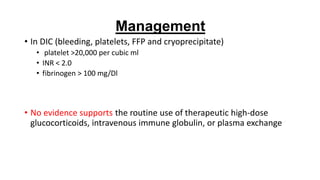
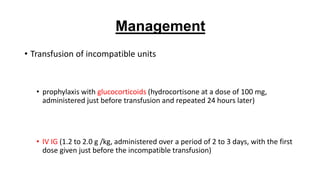
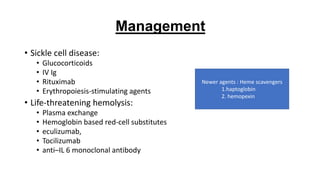
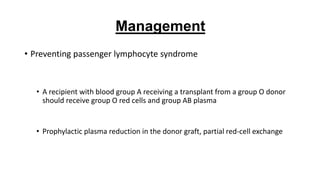
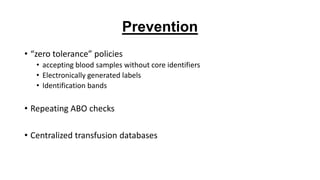
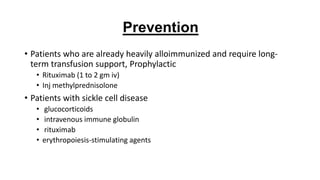
Hemolytic transfusion reactions (HTR) are adverse reactions to blood transfusions that can range from subclinical to lethal. They occur when a patient receives incompatible red blood cells and their immune system mounts an immune response that destroys the transfused red blood cells. The summary discusses preventive strategies like electronic verification systems and protocols to avoid incompatible transfusions, as well as treatments for different types of reactions like acute HTR, delayed HTR, and passenger lymphocyte syndrome in transplant recipients. Effective prevention and management requires understanding the pathophysiology and risk factors for different transfusion reactions.