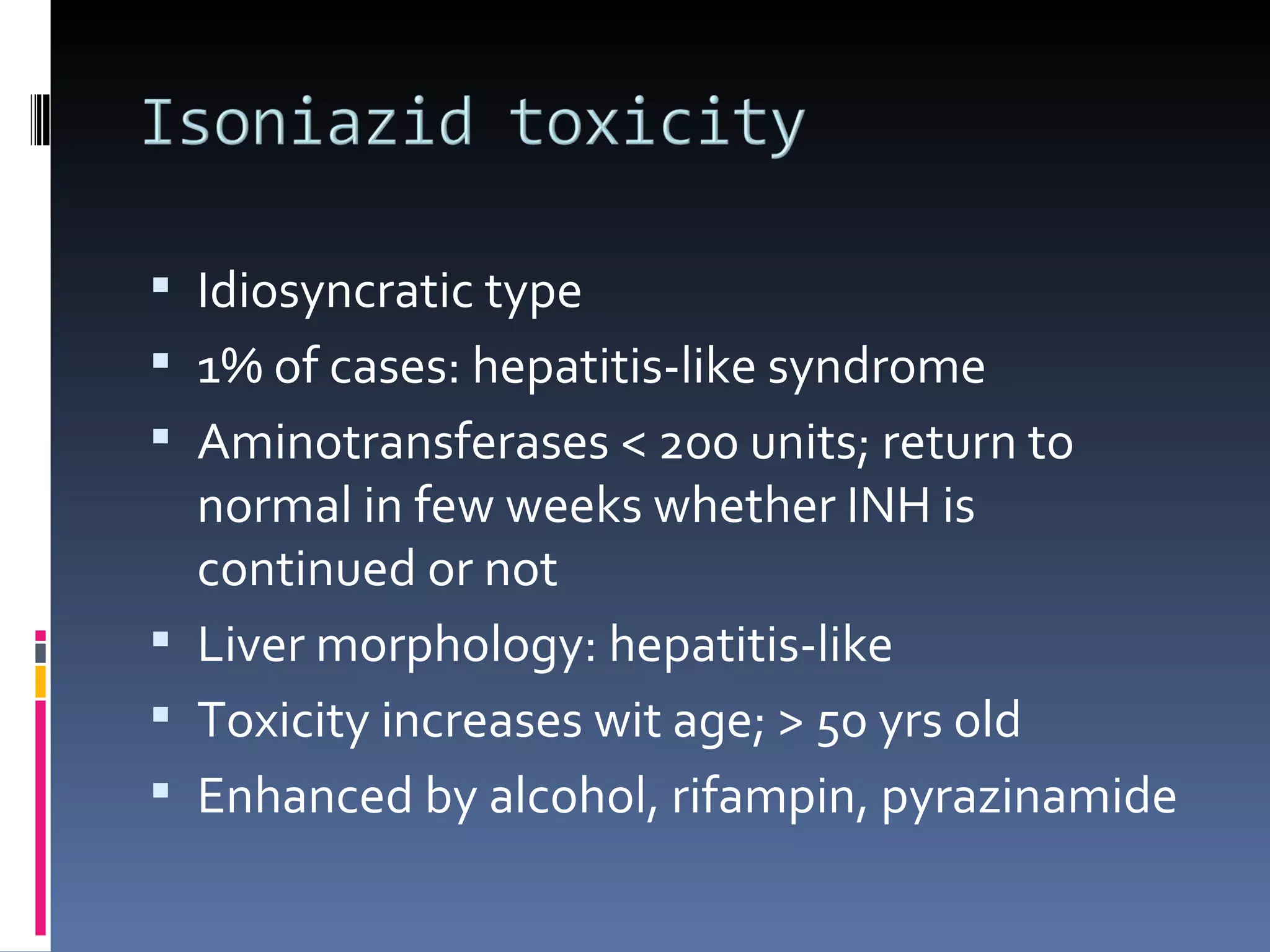
The document discusses various causes of drug-induced liver injury including direct toxicity from drugs like acetaminophen and carbon tetrachloride as well as idiosyncratic reactions. Certain drugs are more likely to cause hepatotoxicity through both direct toxicity and idiosyncratic mechanisms. Supportive treatment measures for acetaminophen overdose-induced liver injury are also outlined. Herbal and dietary supplements can also potentially cause liver injury through mechanisms like pyrrolizidine alkaloid contamination.