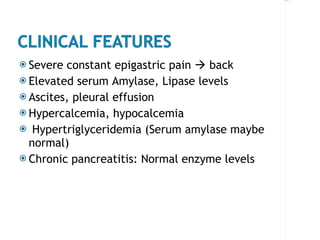
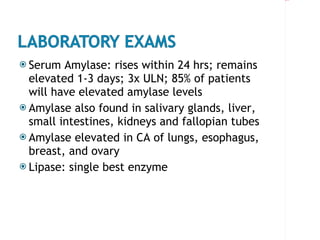
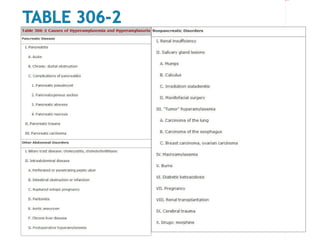
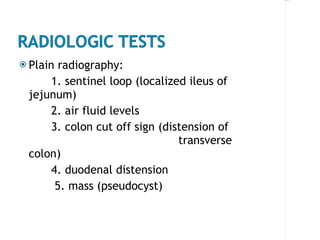
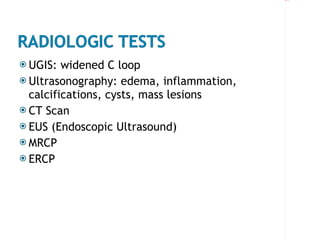
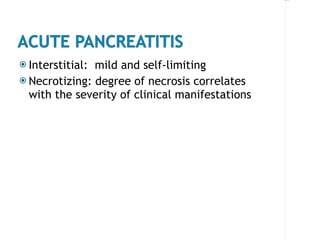
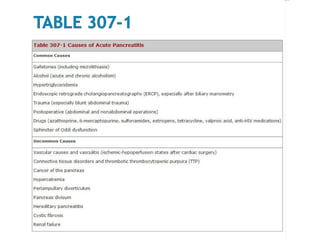
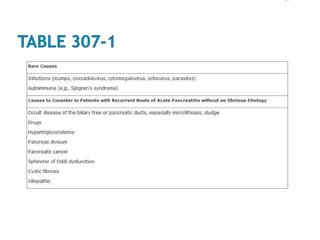
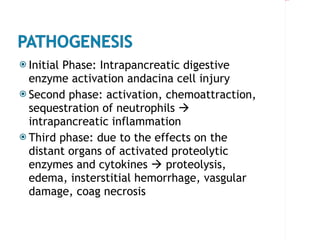
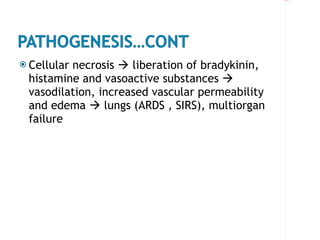
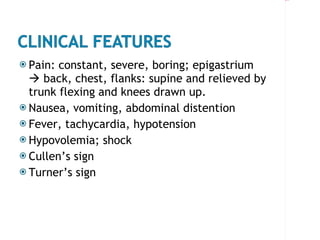
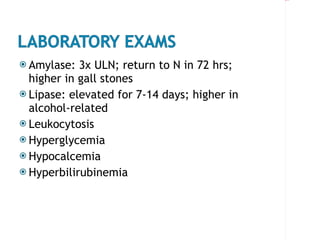
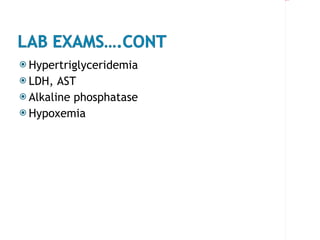
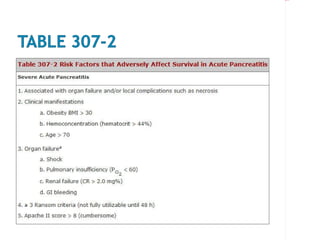
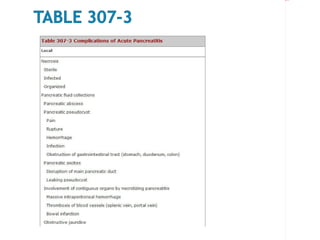
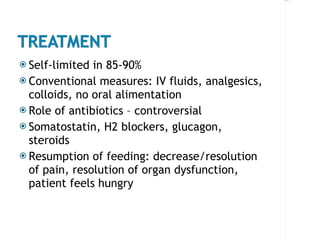
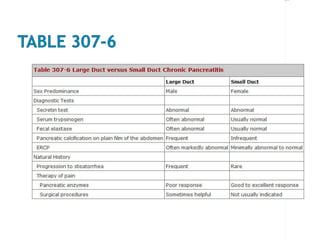
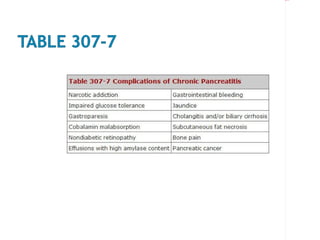
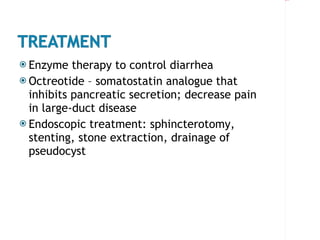
The document discusses acute and chronic pancreatitis, including causes such as alcohol abuse, gallstones, and trauma. It describes clinical features such as severe epigastric pain and elevated serum amylase and lipase levels. Diagnostic tests include blood tests, imaging like CT scans and MRCP, and endoscopic ultrasound. Treatment depends on the severity and includes IV fluids, analgesics, antibiotics, and surgery for complications like pseudocysts or obstruction.