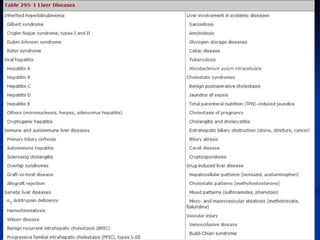
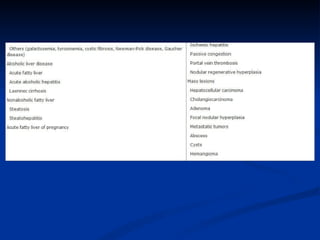
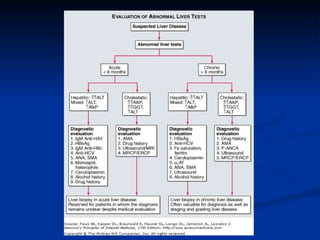
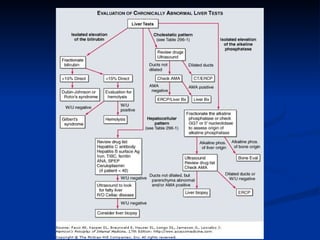
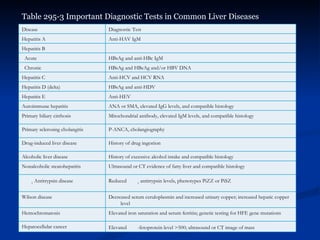
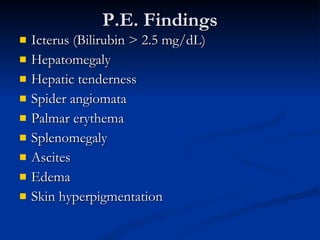
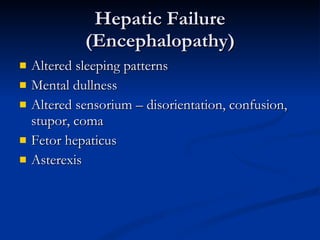
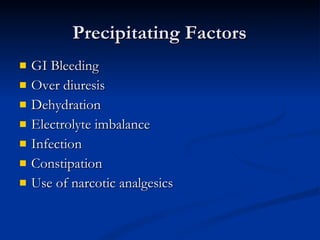
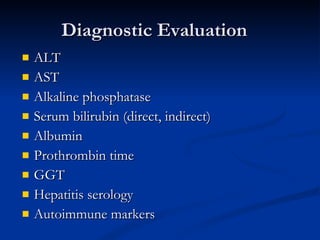
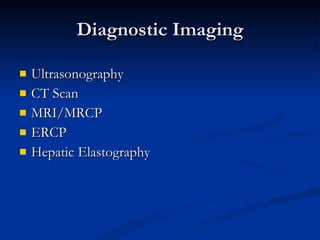
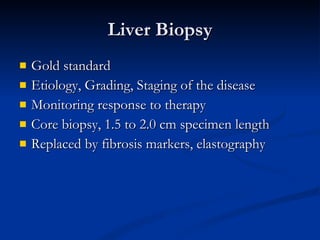
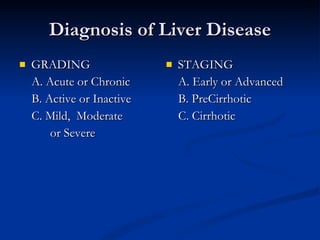
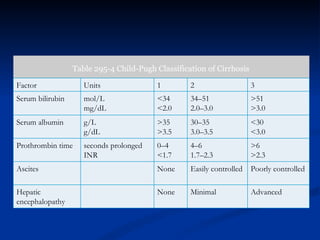
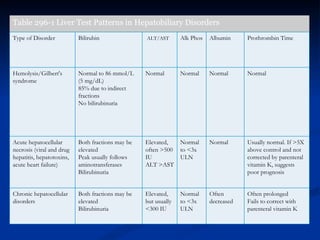
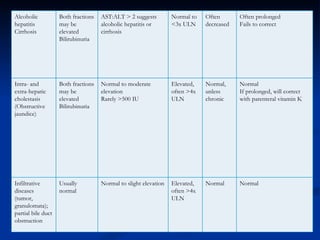
This document provides an overview of evaluating and diagnosing liver disease. It discusses classifying liver diseases as hepatocellular, cholestatic, or mixed based on etiology and evaluating disease severity and stage. Common symptoms, diagnostic tests, clinical findings, and classifications such as Child-Pugh staging for cirrhosis are outlined.