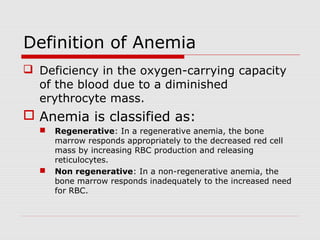
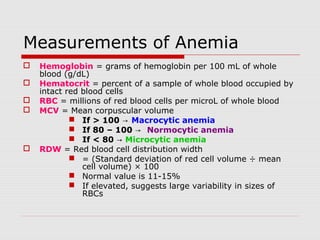
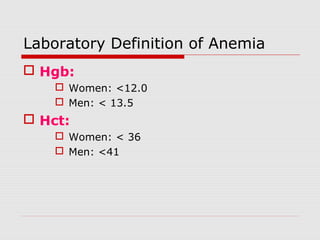
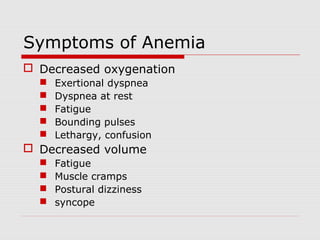
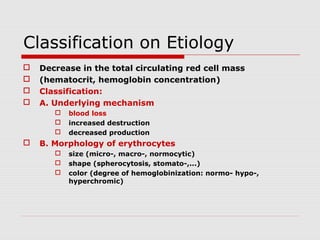
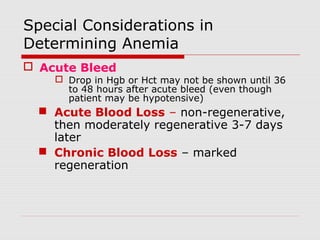
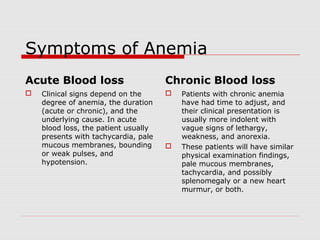
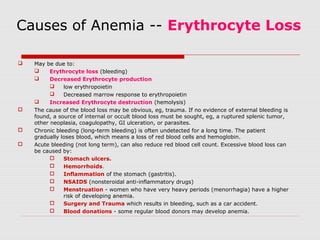
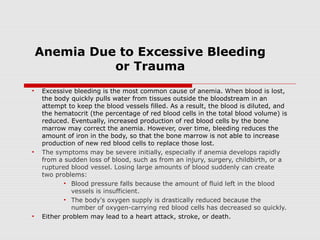
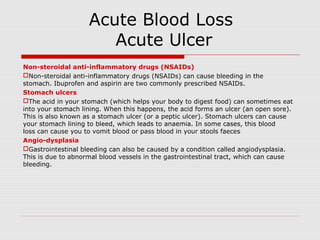
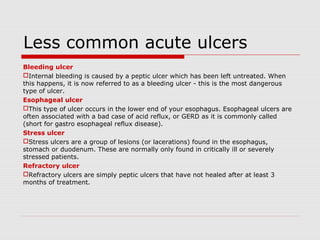
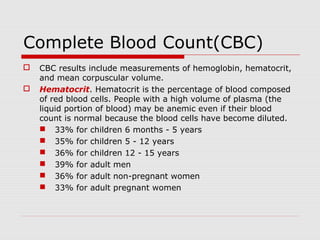
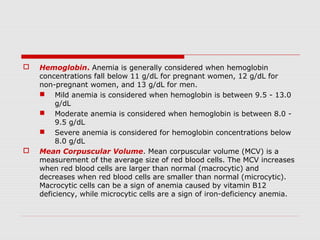
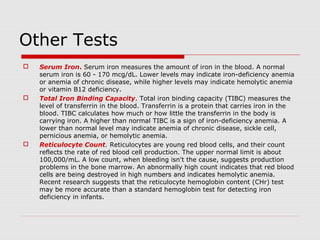
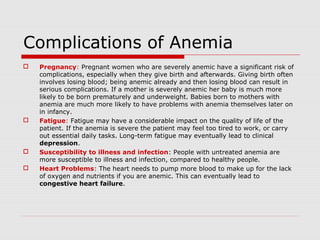
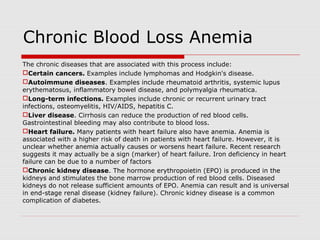
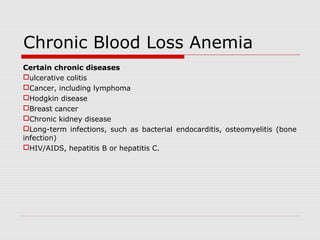
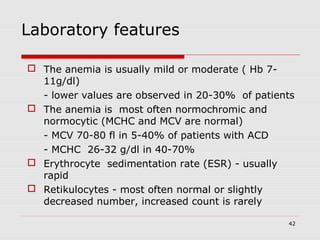
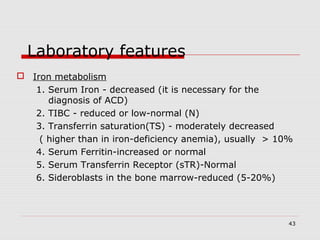
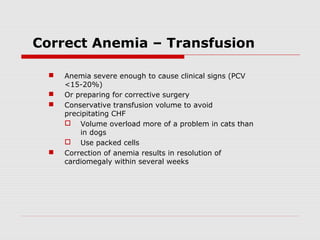
Anemia is defined as a deficiency in oxygen-carrying capacity of the blood due to diminished red blood cells. It is classified as regenerative or non-regenerative based on bone marrow response. Anemia is measured by hemoglobin, hematocrit, red blood cell count, mean corpuscular volume, and red cell distribution width. Symptoms include fatigue, dizziness, and shortness of breath. Causes include blood loss, increased destruction, or decreased production. Chronic ulcers like venous and diabetic ulcers account for most cases and result from prolonged pressure or reduced blood flow to tissues.