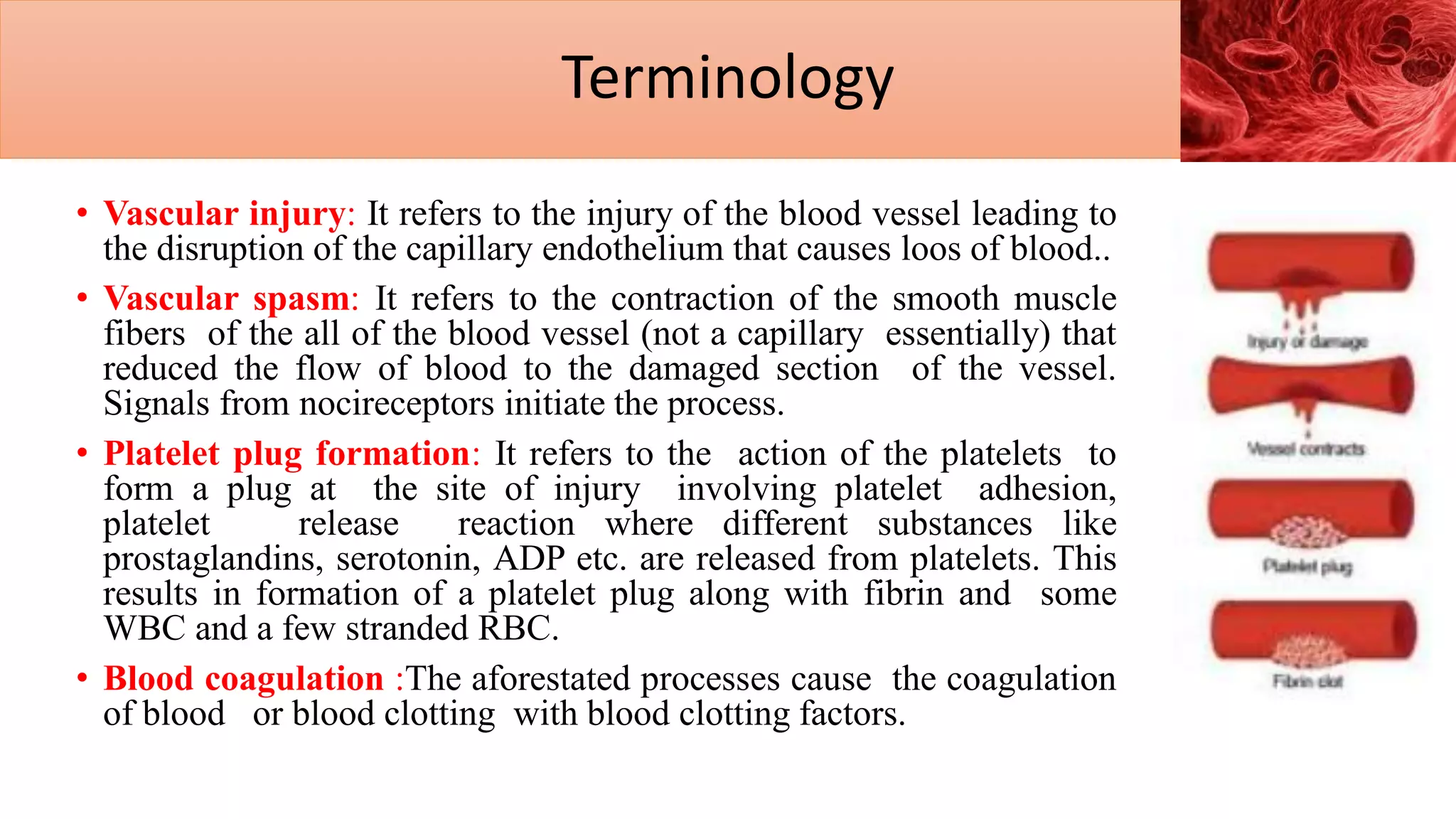
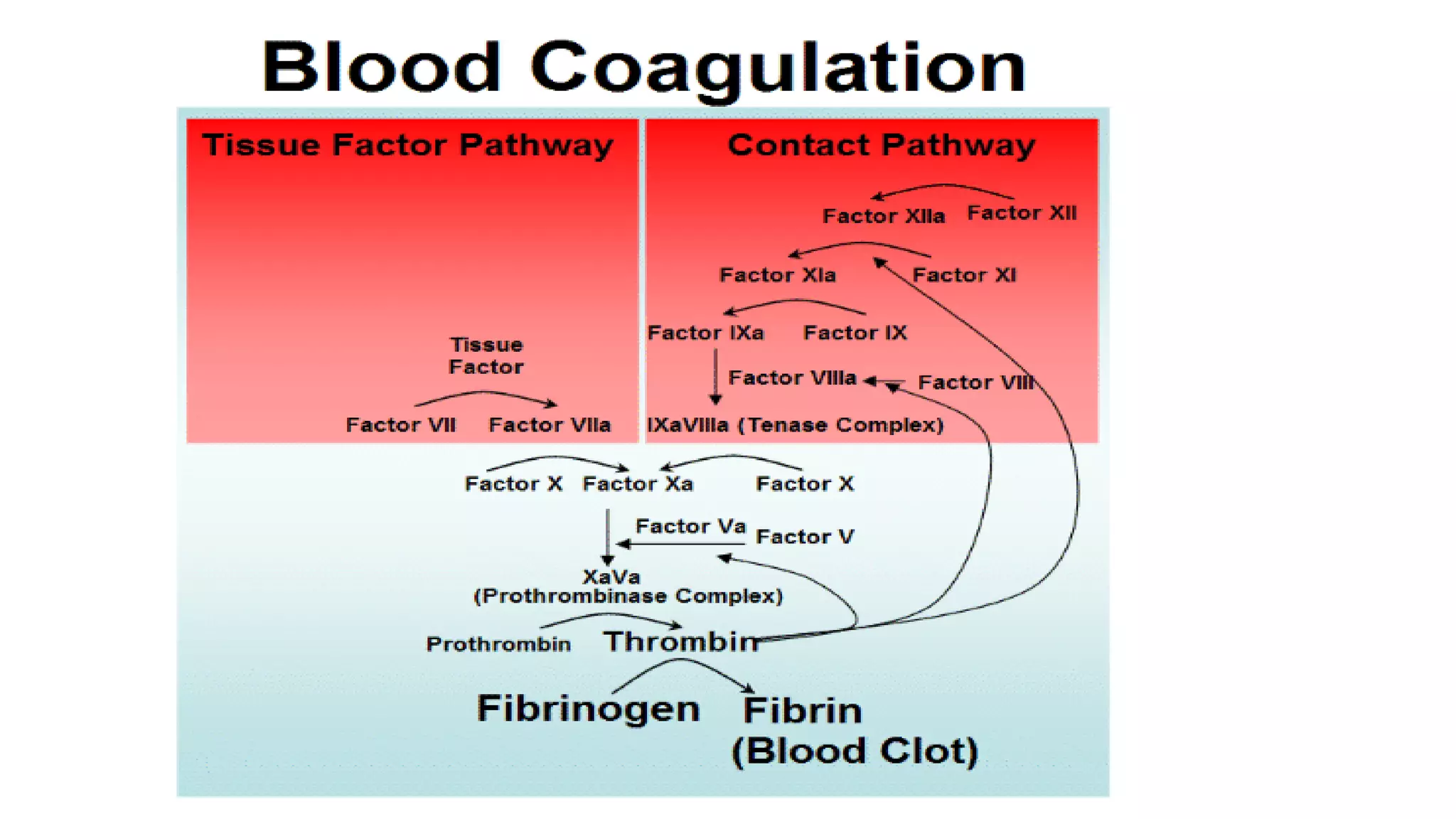
Blood coagulation, or clotting, is a crucial process that prevents excessive bleeding when blood vessels are injured, involving platelets and plasma proteins. Hemostasis consists of three main steps: vasoconstriction, platelet plug formation, and blood coagulation, leading to wound healing. Key components such as platelet activation and clotting factors facilitate the transition from liquid blood to a solid clot, which helps seal the injury until tissue repair occurs.