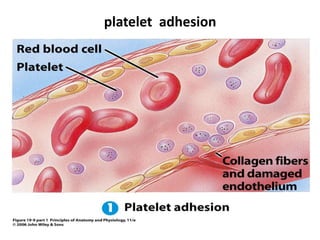
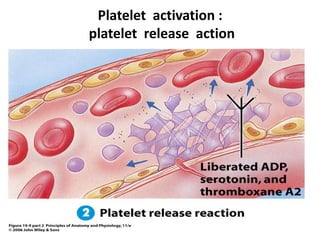
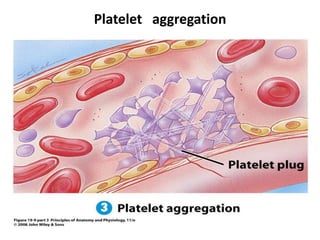
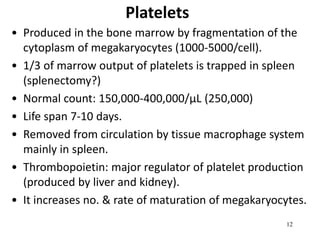
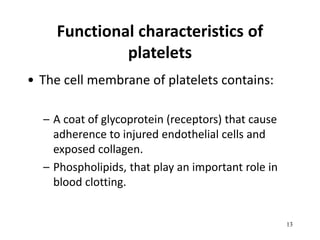
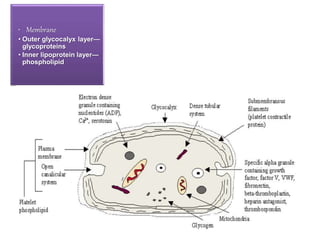
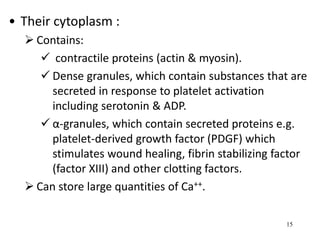
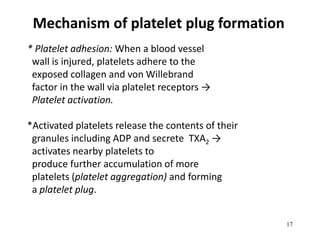
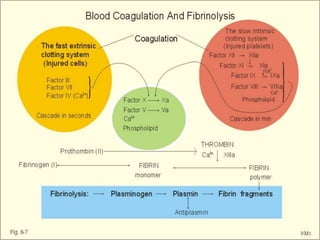
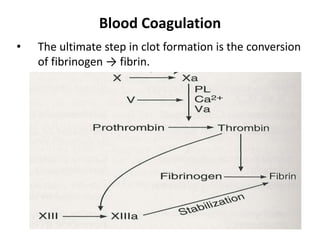
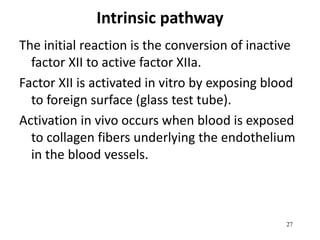
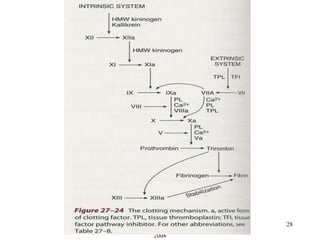
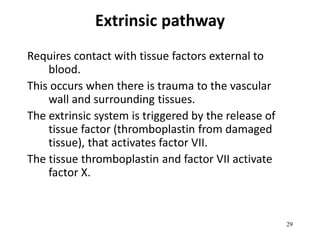
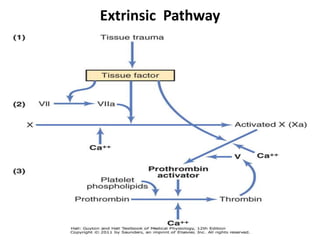
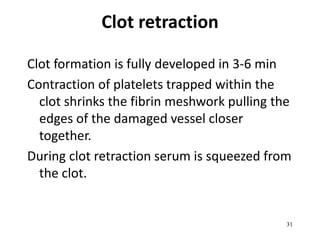
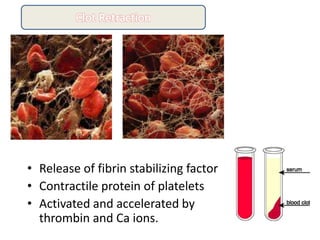
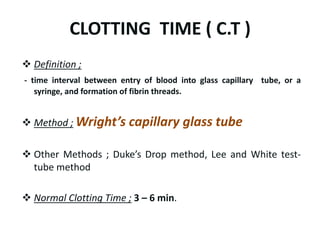
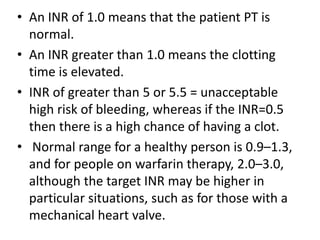
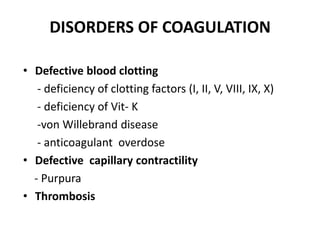
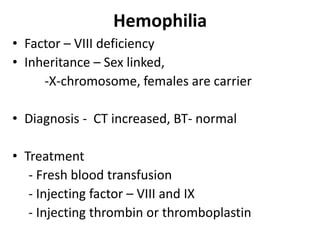
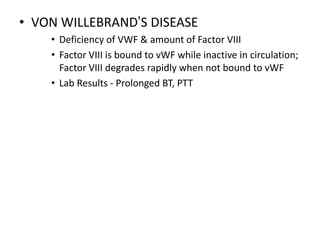
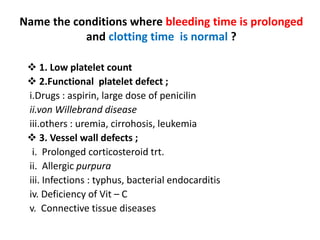
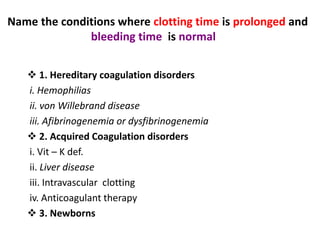
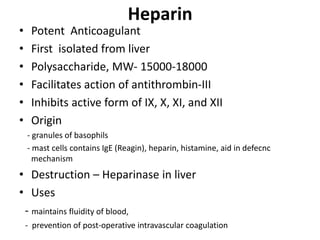
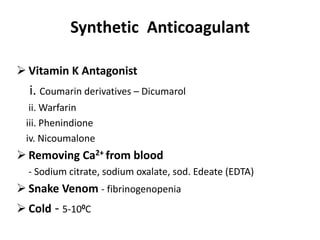
This document summarizes blood coagulation and hemostasis. It discusses platelets, the platelet plug formation process, and the intrinsic and extrinsic pathways of blood coagulation. Disorders of coagulation covered include hemophilia A/B/C, von Willebrand disease, and purpura. Tests of hemostatic function like bleeding time, clotting time, and prothrombin time are also outlined. Anticoagulants like heparin and warfarin are briefly described.