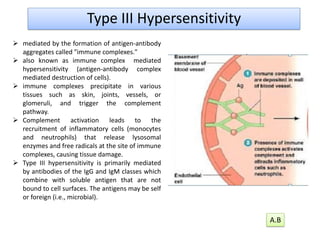
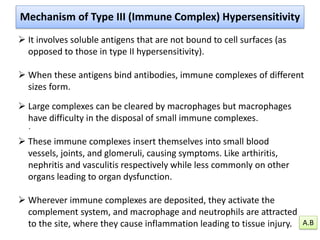
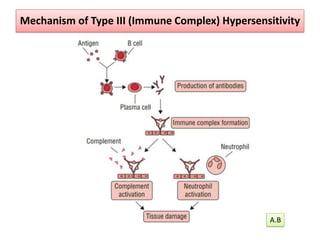
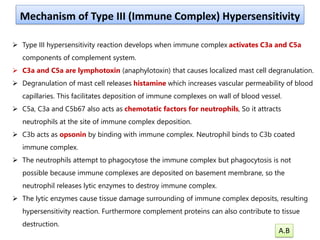
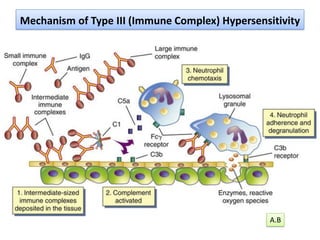
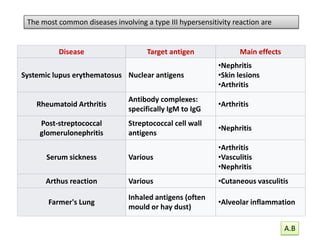
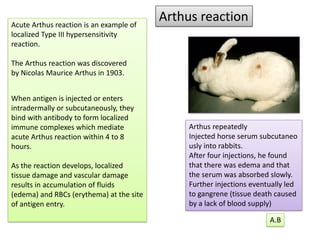
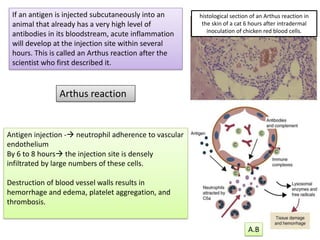
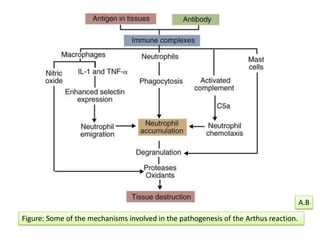
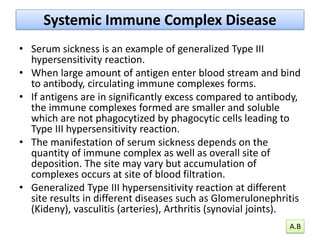
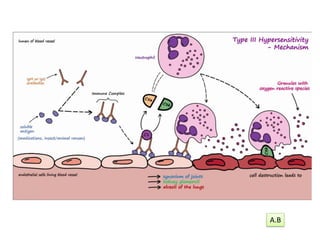
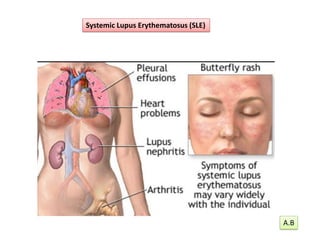
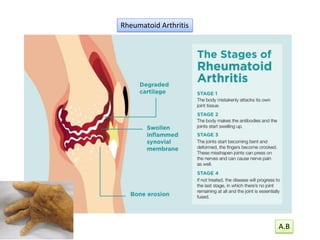
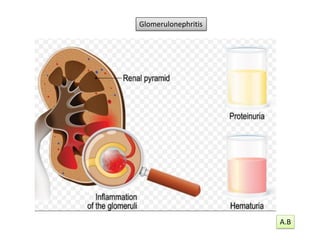
Type III hypersensitivity, also known as immune complex-mediated hypersensitivity, occurs when antigen-antibody complexes precipitate in tissues, leading to inflammation and tissue damage via complement activation and cell recruitment. It is primarily mediated by IgG and IgM antibodies against soluble antigens and can result in various conditions such as systemic lupus erythematosus, rheumatoid arthritis, and post-streptococcal glomerulonephritis. The two main forms are localized reactions (arthus reaction) and generalized reactions (serum sickness), characterized by different immune complex responses and resulting symptoms.