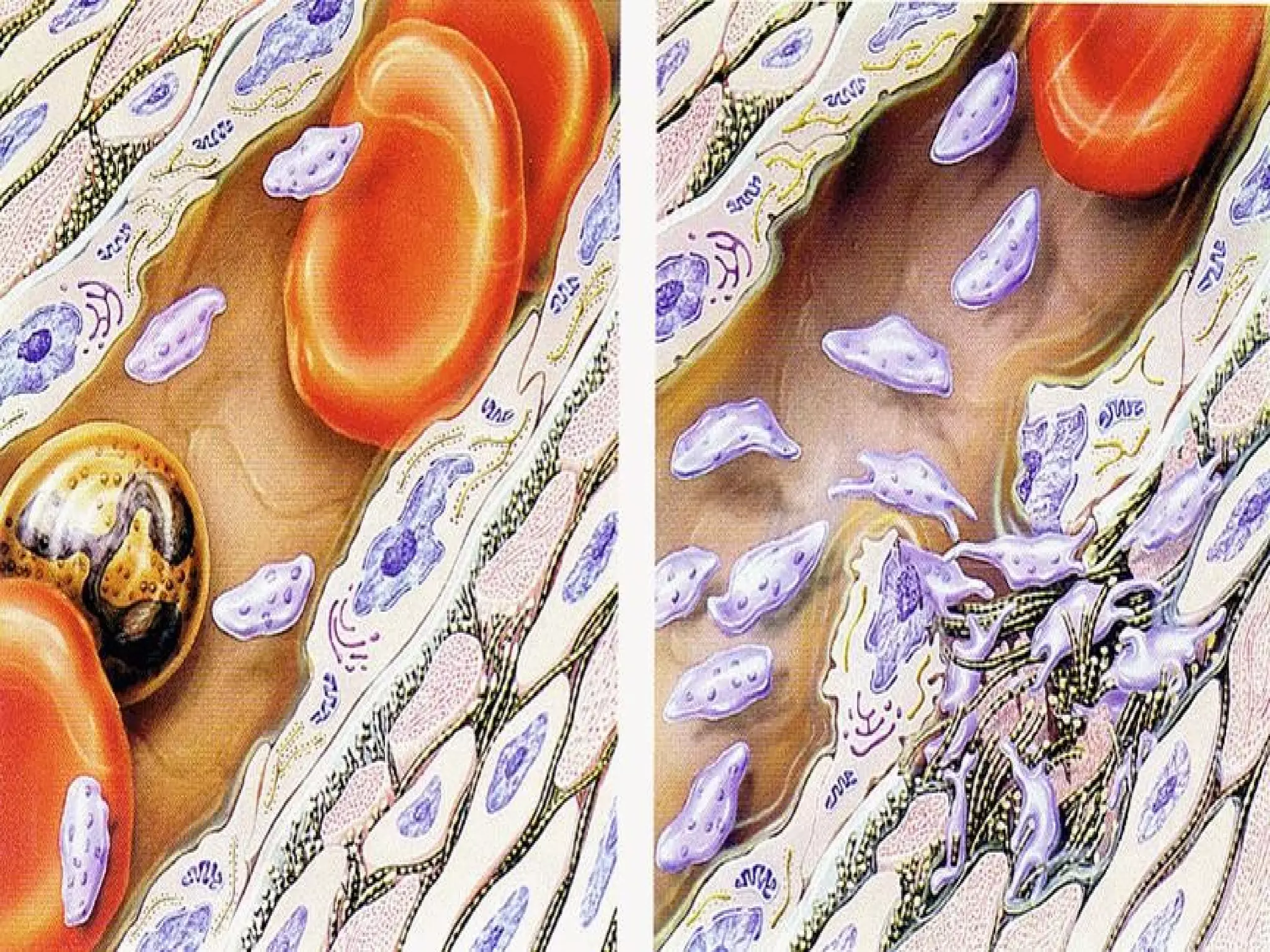
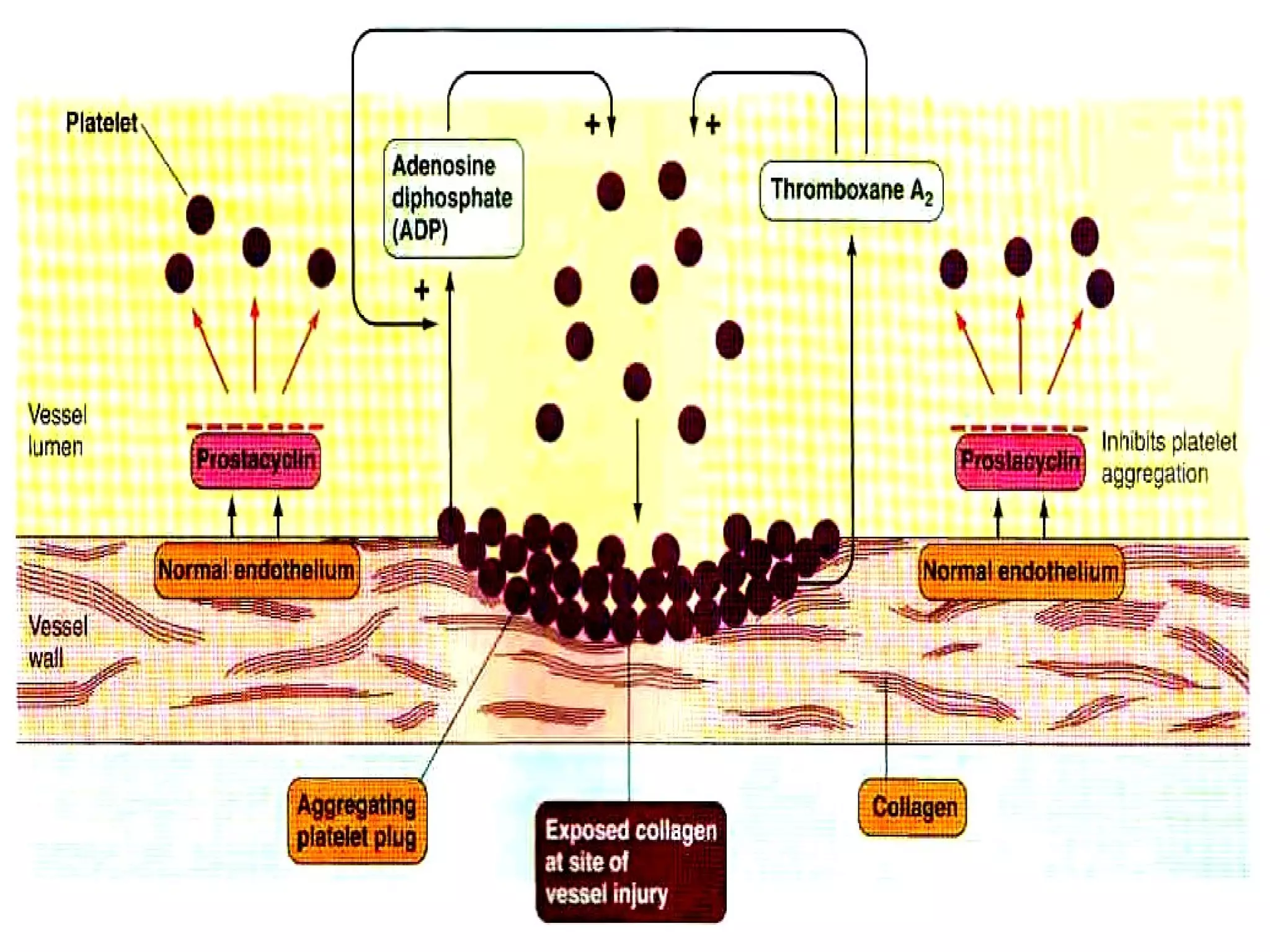
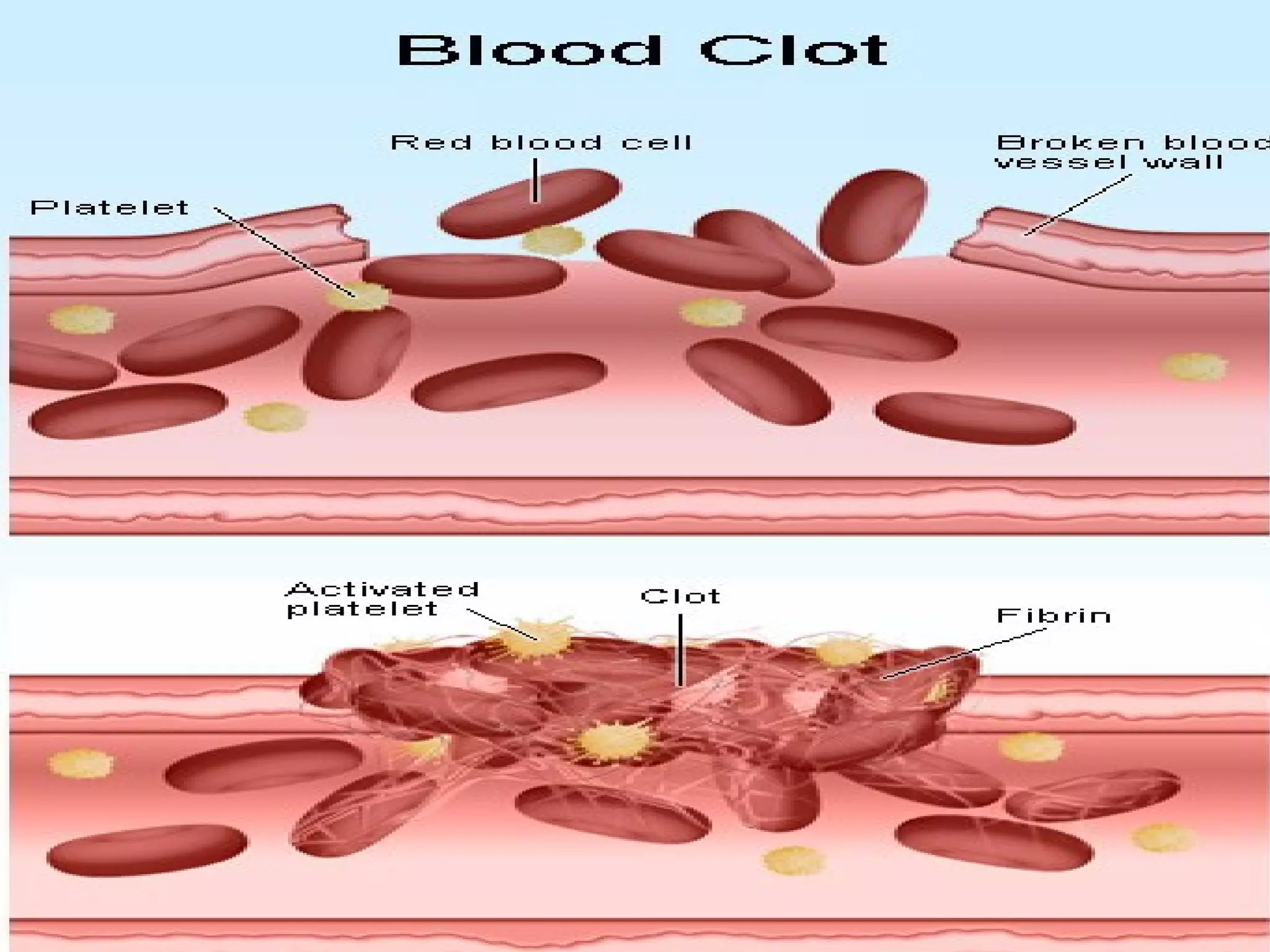
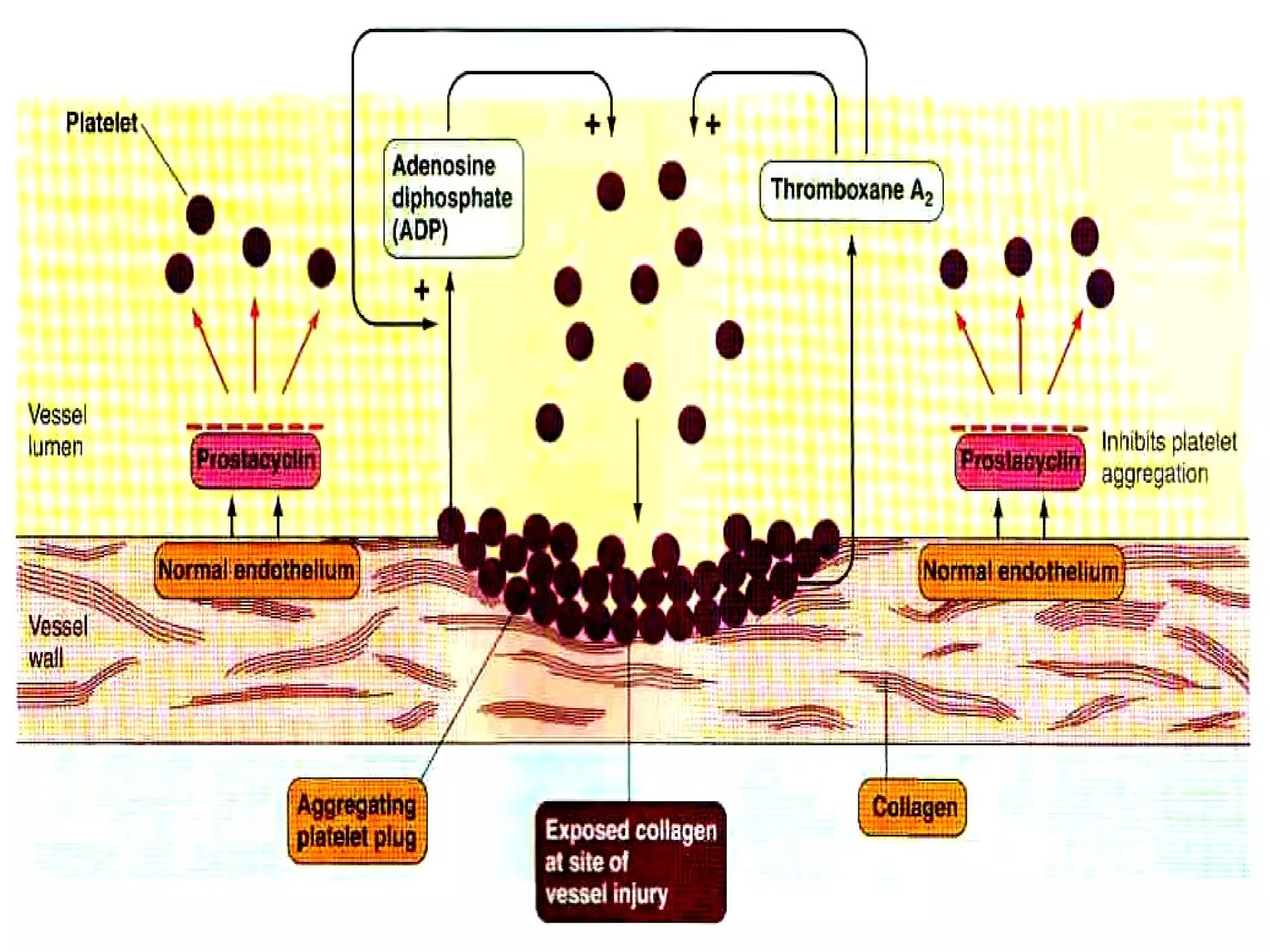
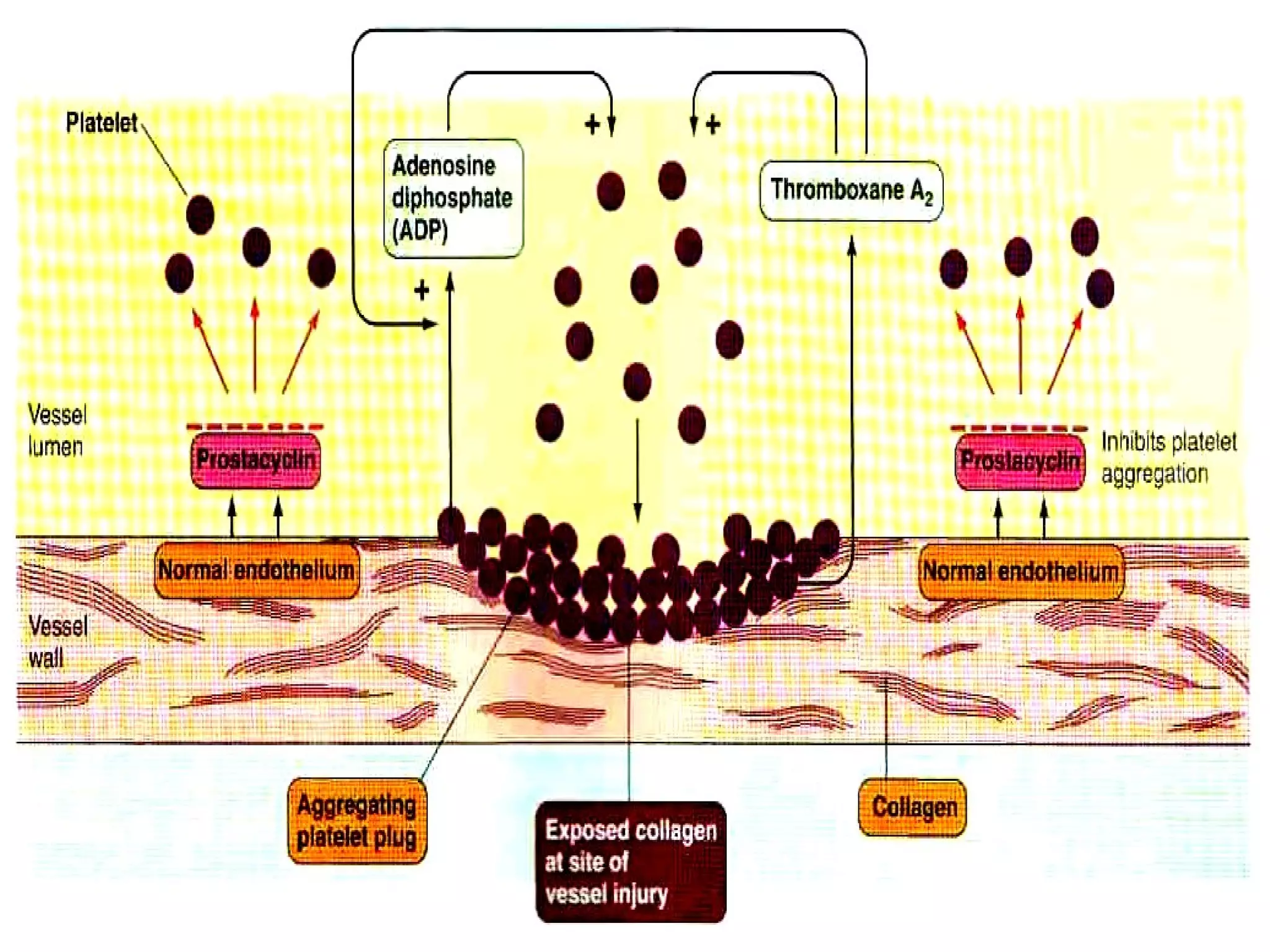
Hemostasis is the prevention of blood loss from ruptured blood vessels. It involves three key events: 1) vascular constriction to reduce blood flow, 2) formation of a platelet plug to seal the rupture, and 3) formation of a blood clot through coagulation to reinforce the seal. Platelets adhere to collagen at the rupture site and aggregate, releasing chemicals to recruit more platelets until the plug is formed. Meanwhile, coagulation factors in the blood activate in a cascade, ultimately converting fibrinogen to fibrin fibers that strengthen the platelet plug and form a clot. The clot or plug then either organizes into fibrous tissue to permanently close the rupture or dissolves if no longer needed.