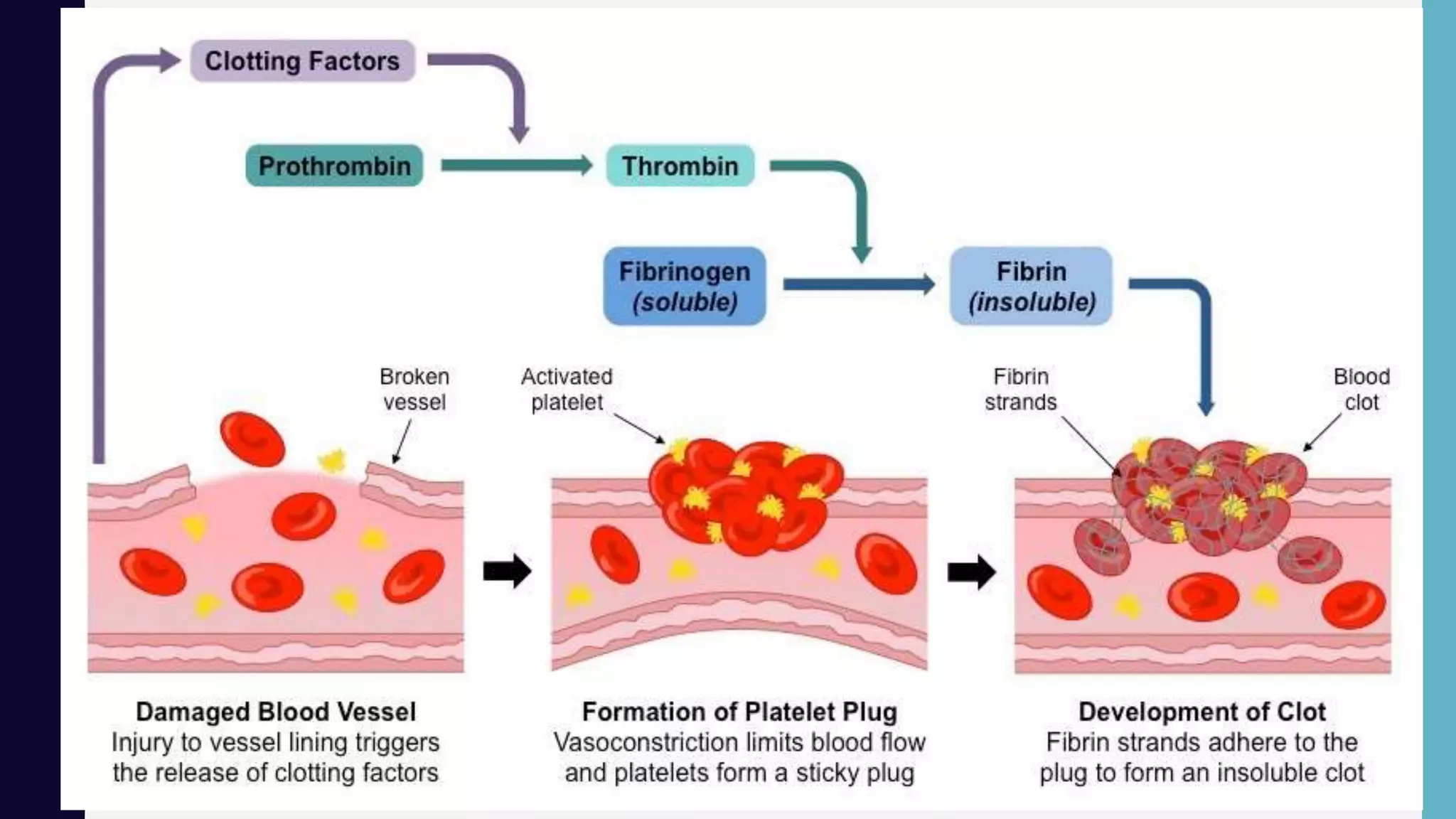
Hemostasis is the process by which bleeding is stopped through a complex cascade of interlinked steps, culminating in the formation of a blood clot. This involves initial platelet aggregation and vasoconstriction to form a temporary plug, followed by activation of coagulation factors that trigger the production of fibrin strands surrounding the platelet plug to form a stable clot. Precise control of coagulation prevents blood loss from injury while maintaining blood fluidity throughout the uninjured circulatory system.