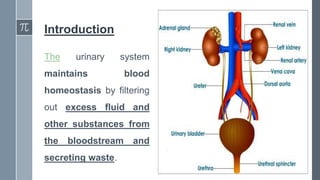
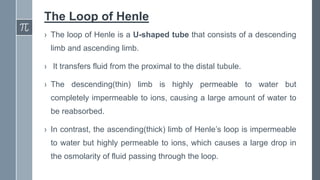
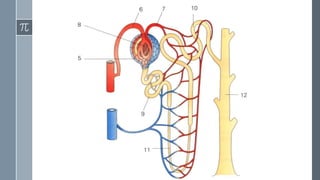
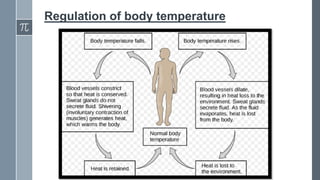
The document provides information about the excretory/renal system. It discusses the key parts of the system including the kidneys, ureters, bladder and urethra. The kidneys filter waste from the blood and regulate fluid levels and electrolyte balance. Key structures within the kidneys are described like nephrons, which are the functional filtering units. Processes like filtration, reabsorption and secretion are explained in how the kidneys form and regulate urine composition. Learning objectives are also outlined to characterize each part's role and illustrate the kidney's microscopic and macroscopic structures.