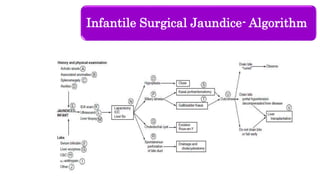
Biliary atresia is a serious condition causing obstruction of bile ducts in infants, leading to cholestasis and potentially liver failure if untreated. The document outlines the etiology, clinical features, diagnostic methods, treatment options, and outcomes of biliary atresia, emphasizing the need for early recognition and surgical intervention to improve prognosis. Surgical options include Kasai's portoenterostomy, and the long-term outlook varies significantly based on age at surgery and post-operative complications.