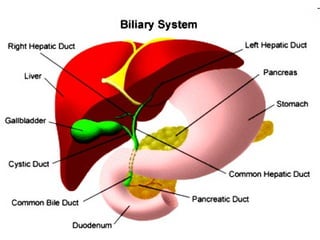
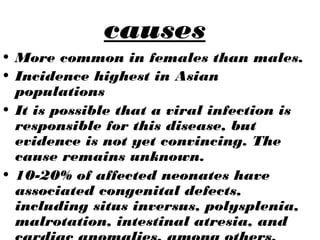
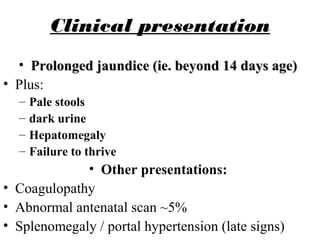
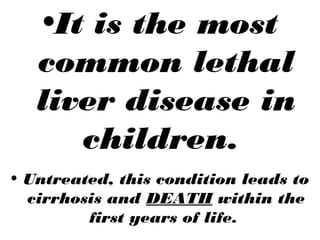
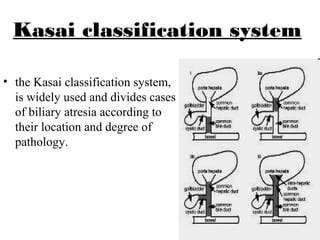
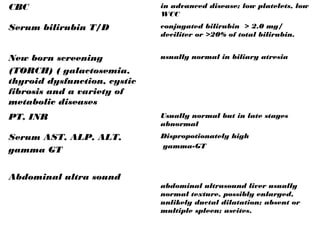
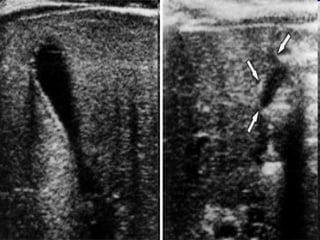
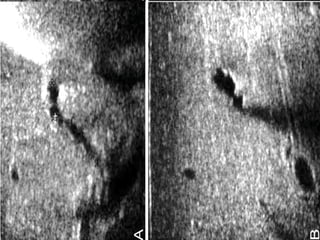
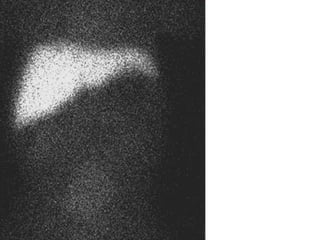
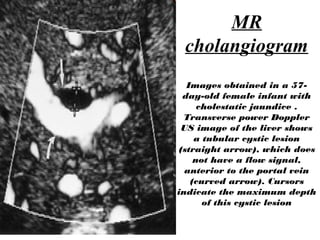
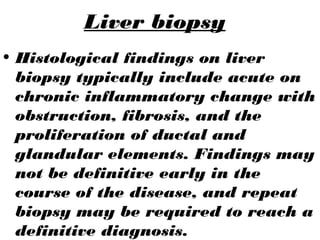
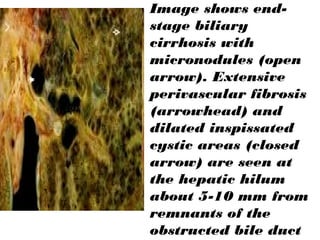
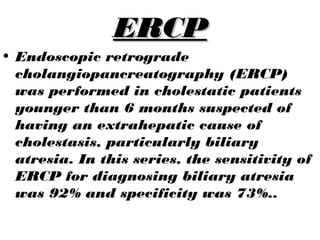
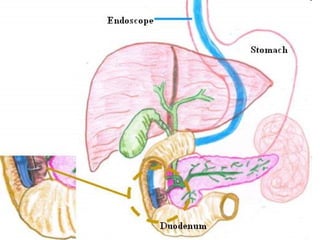
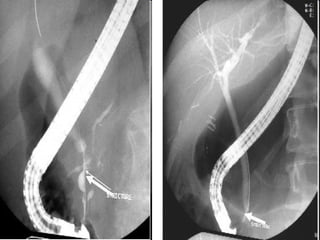
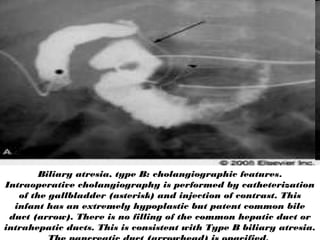
Biliary atresia is a rare disease where the bile ducts outside and inside the liver are destroyed, preventing bile from draining from the liver to the intestines. This leads to jaundice, liver damage, and life-threatening cirrhosis if left untreated. The cause is unknown but may involve a viral infection. Affected infants show prolonged jaundice beyond 14 days of age. Diagnosis involves blood tests, imaging like ultrasound and MRCP, and liver biopsy to examine duct proliferation and fibrosis. The definitive diagnosis is made during surgery using intraoperative cholangiography. Early diagnosis is important so the bile ducts can be surgically reconstructed to drain bile before irreversible liver damage occurs.