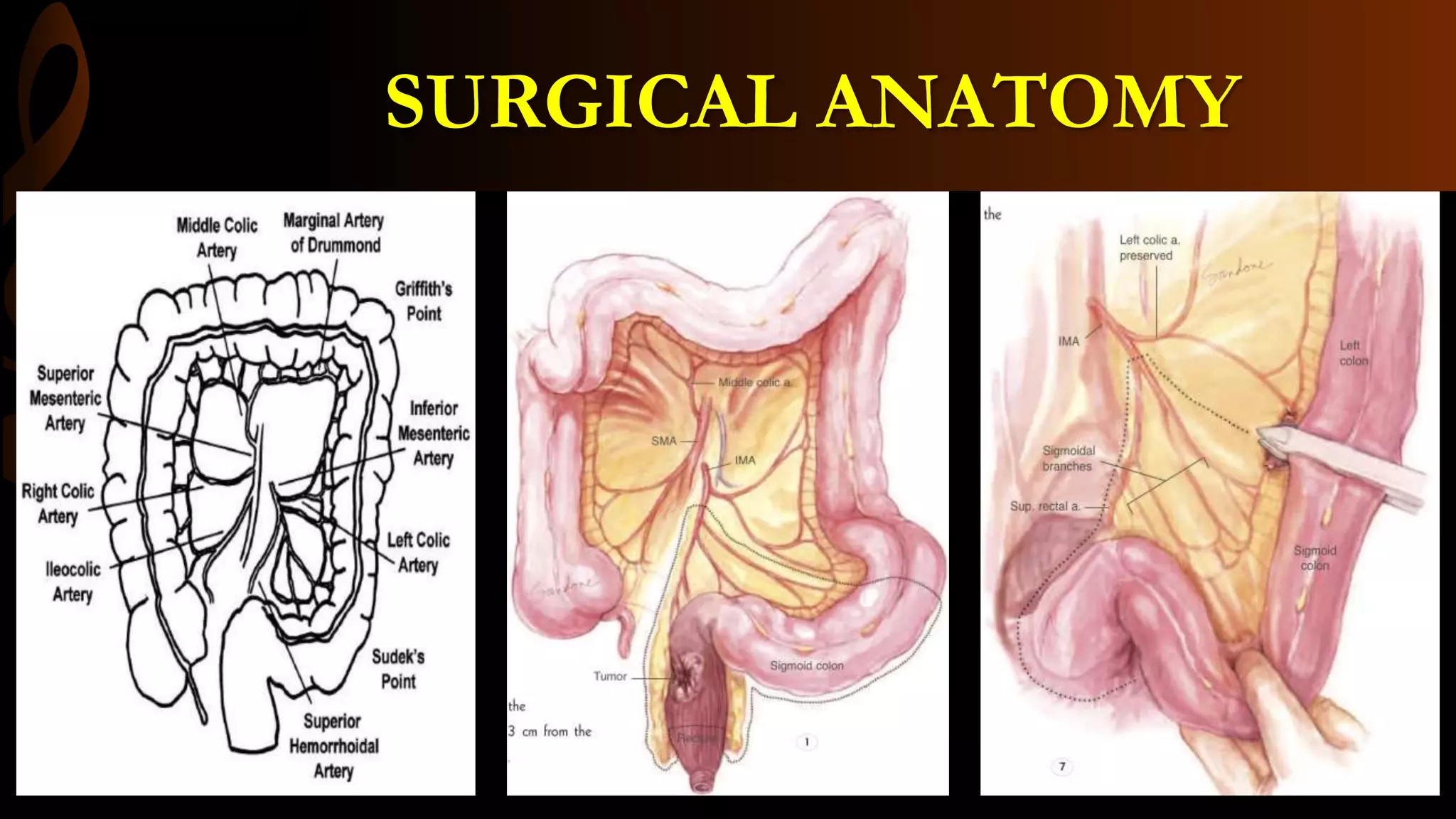
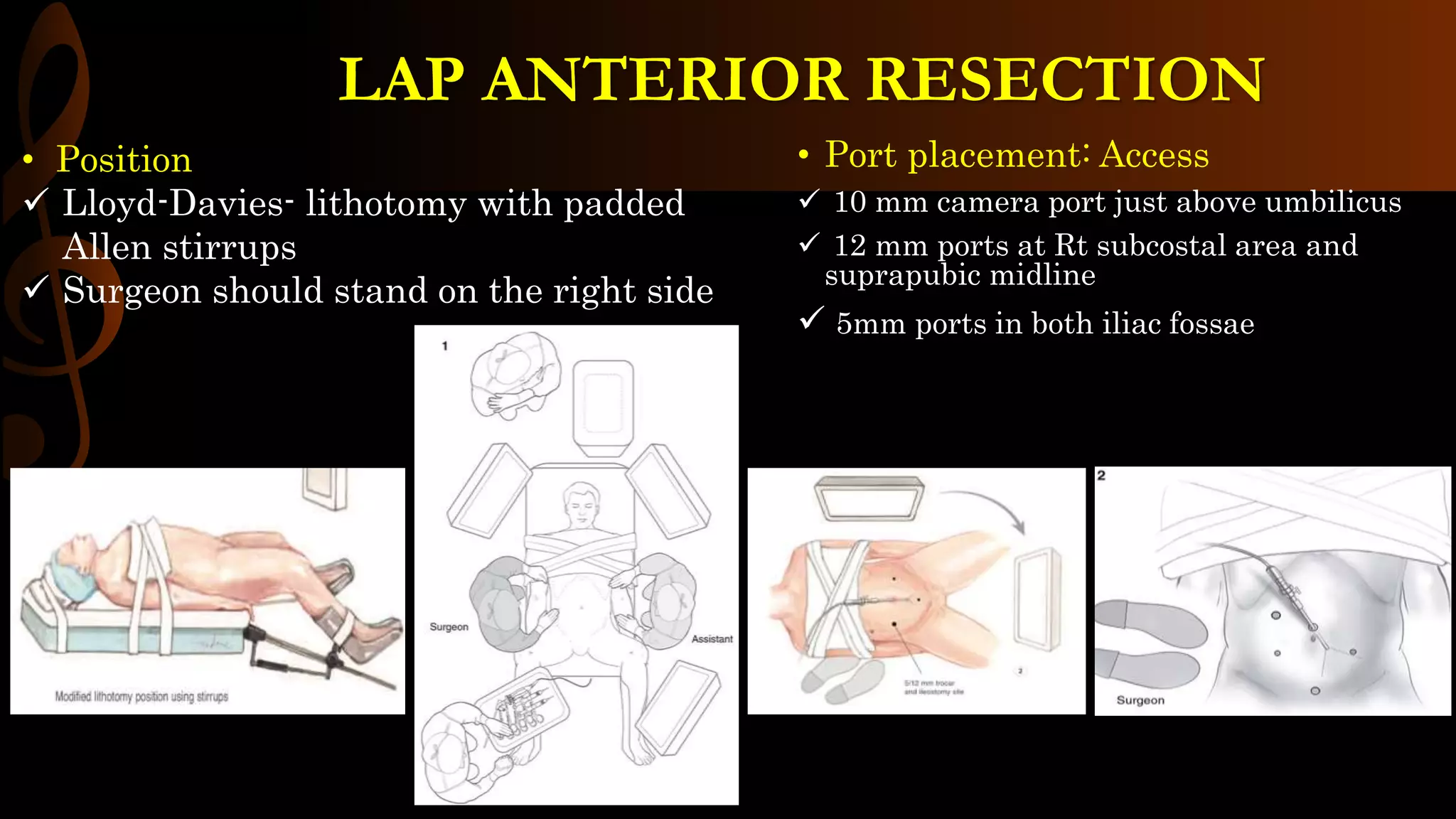
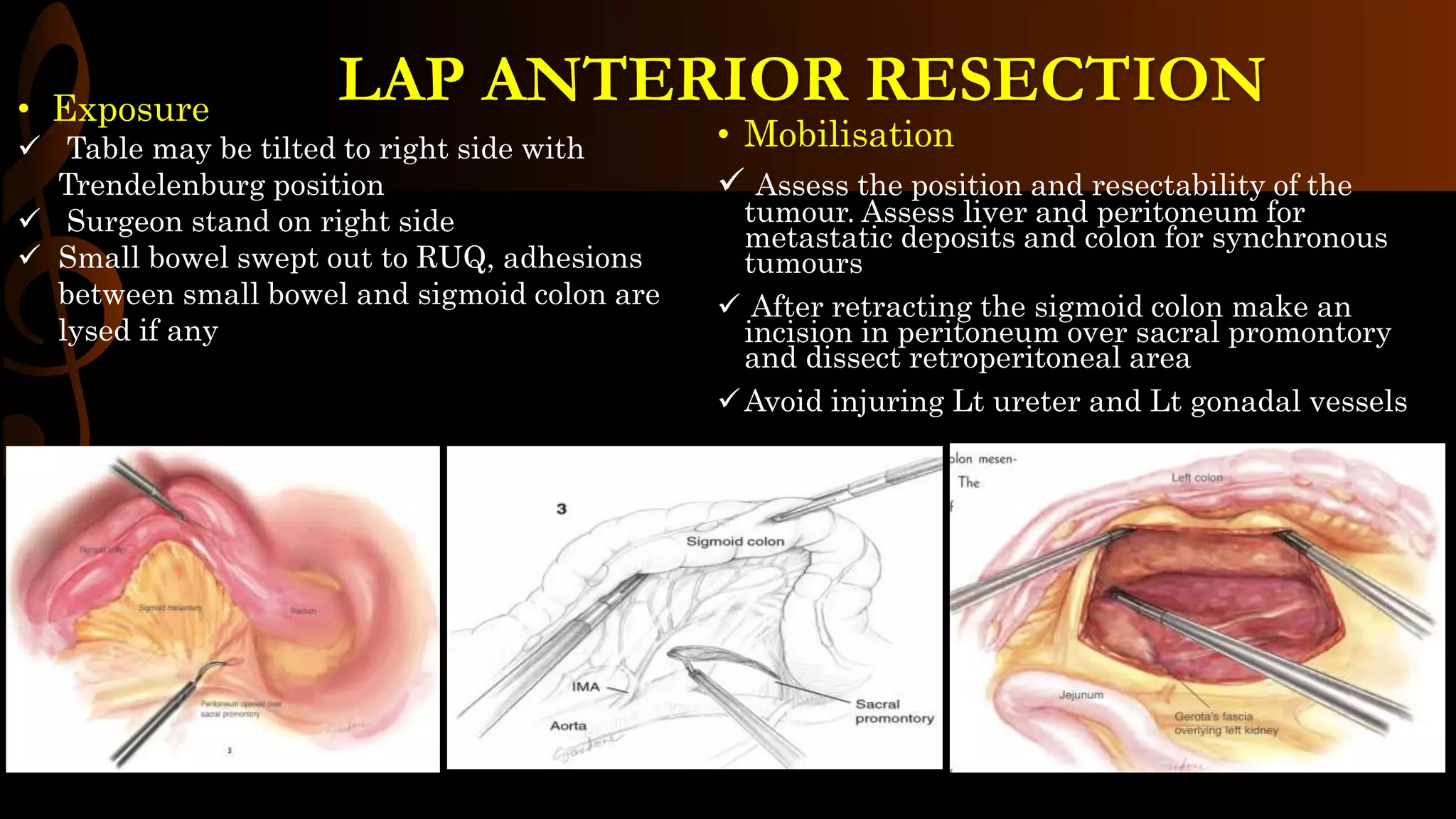
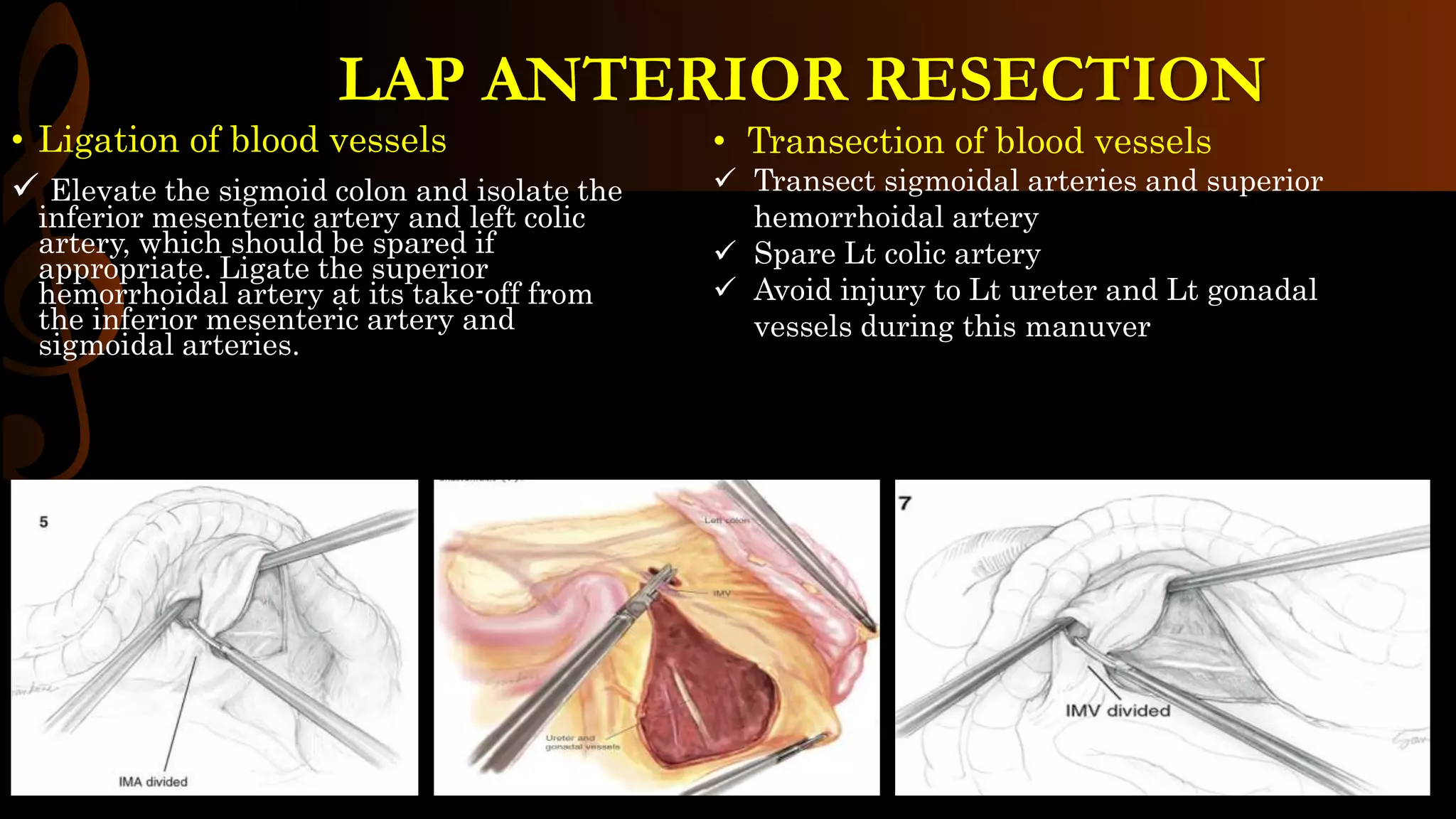
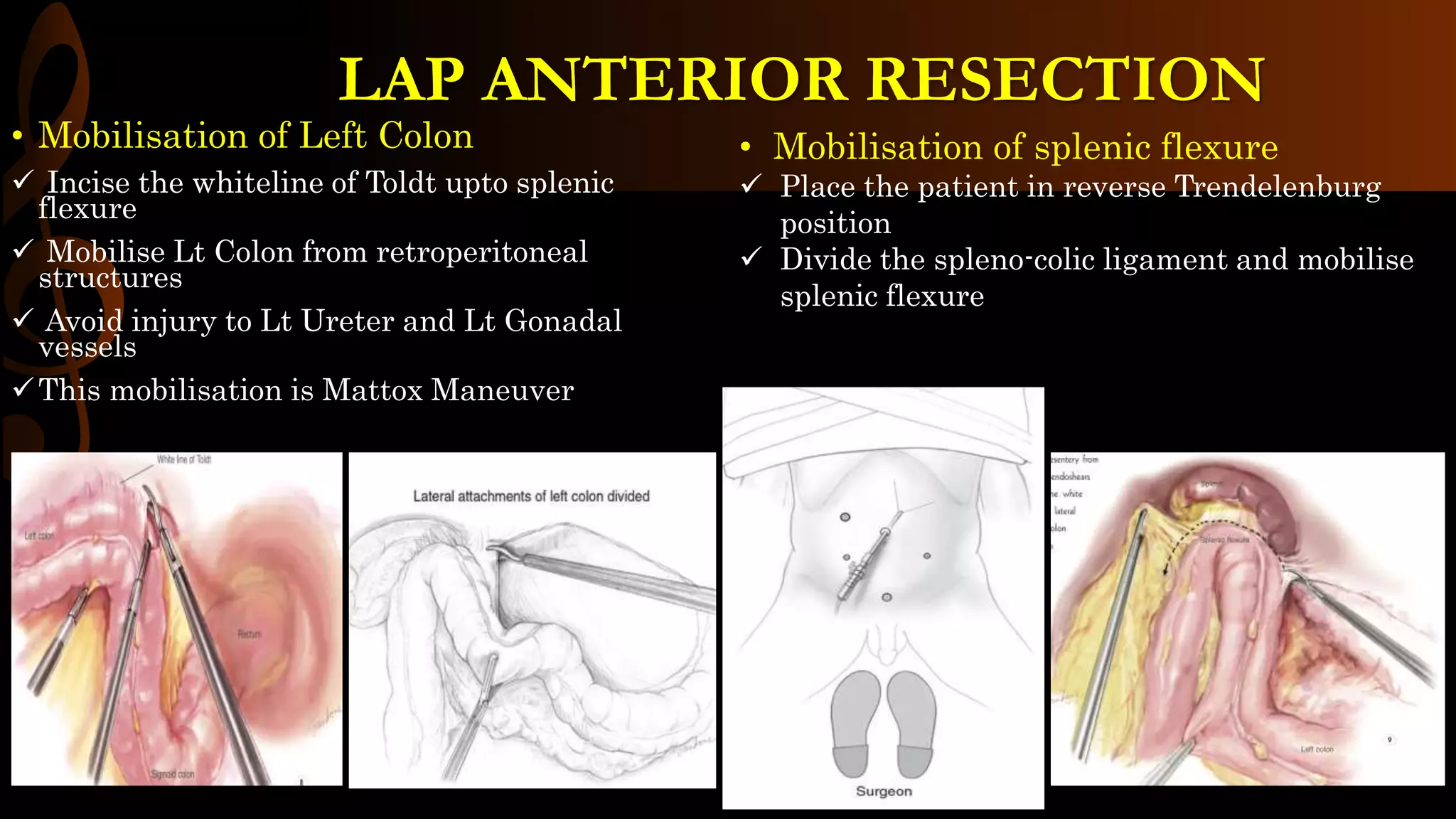
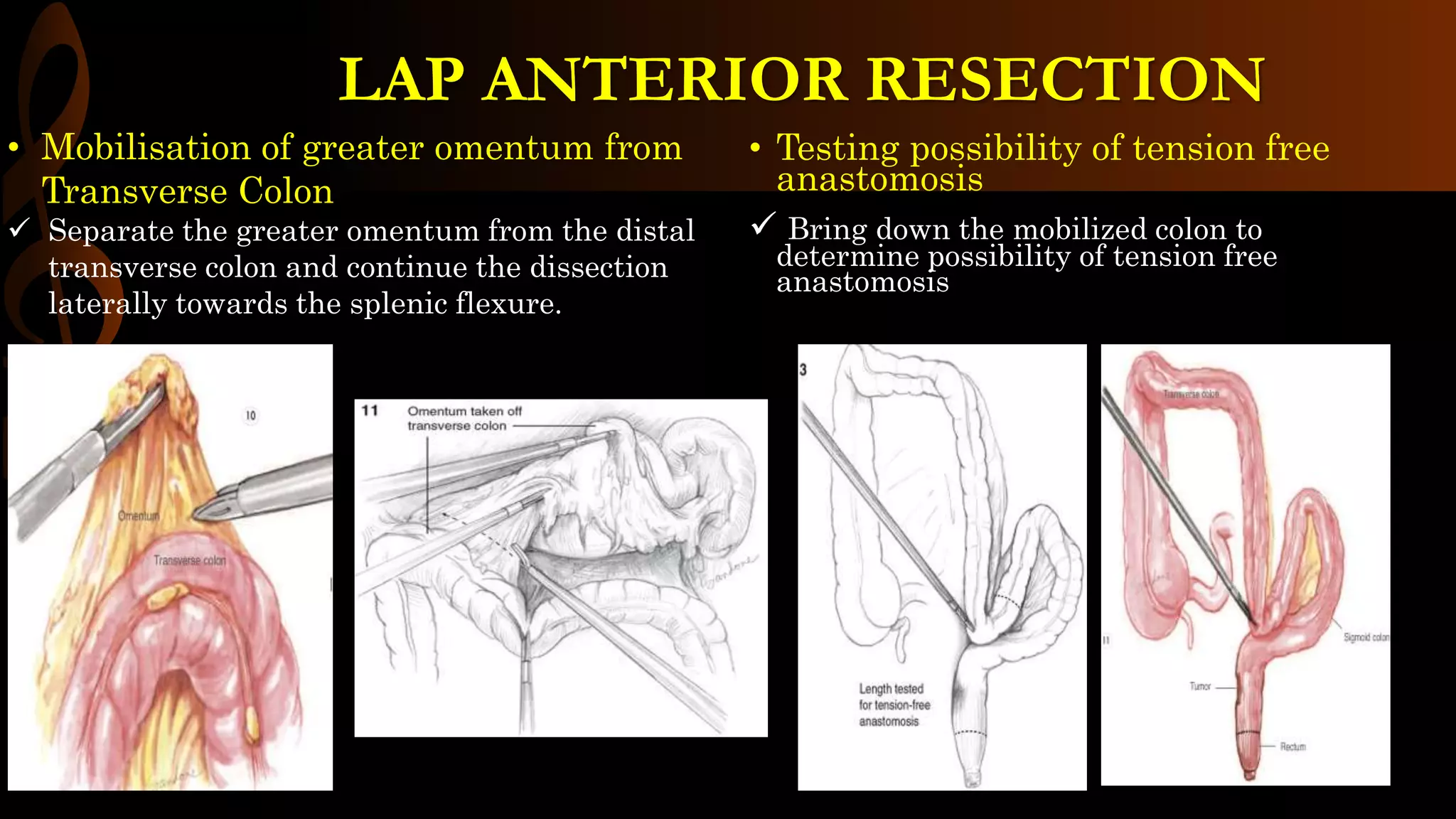
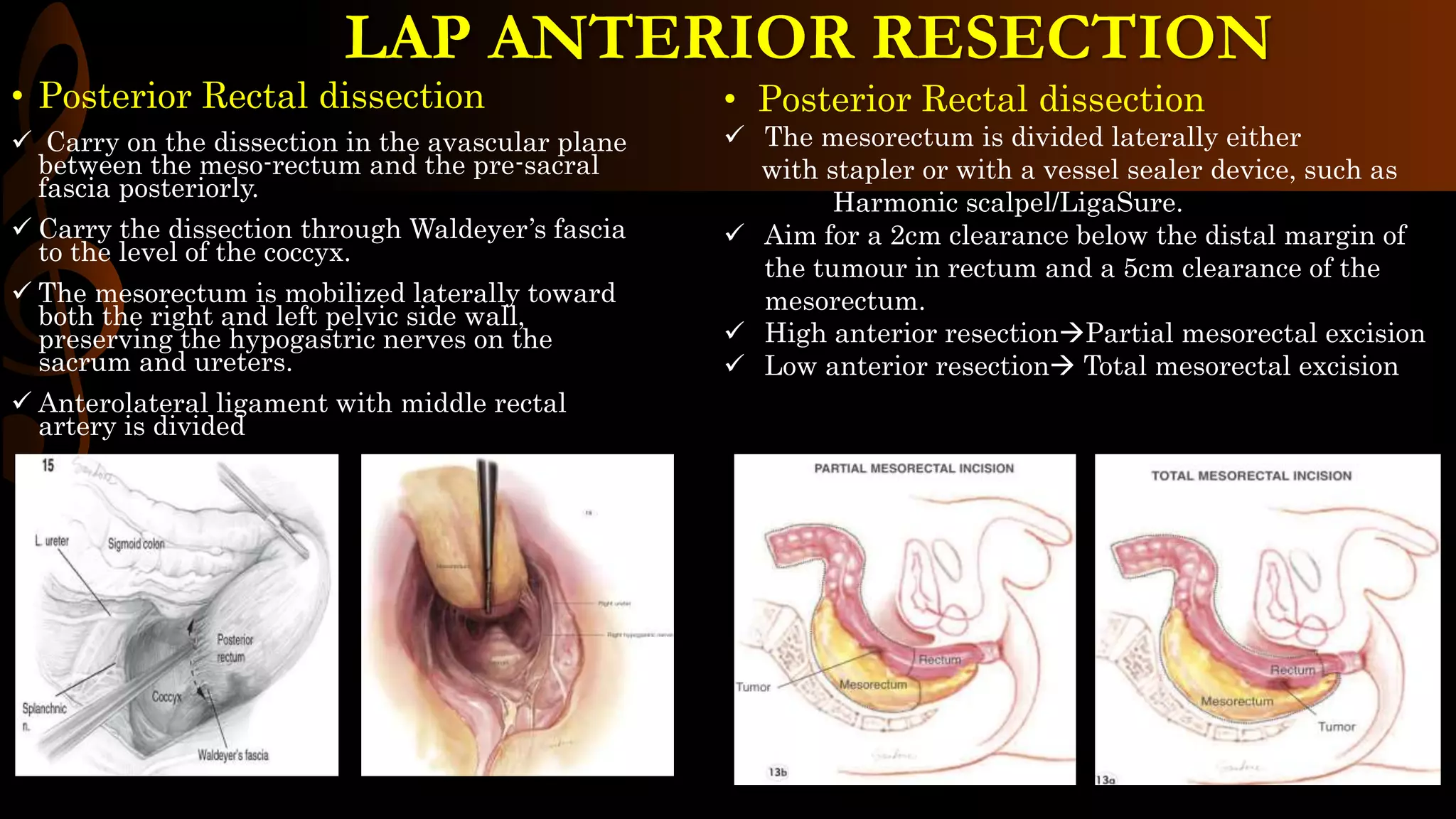
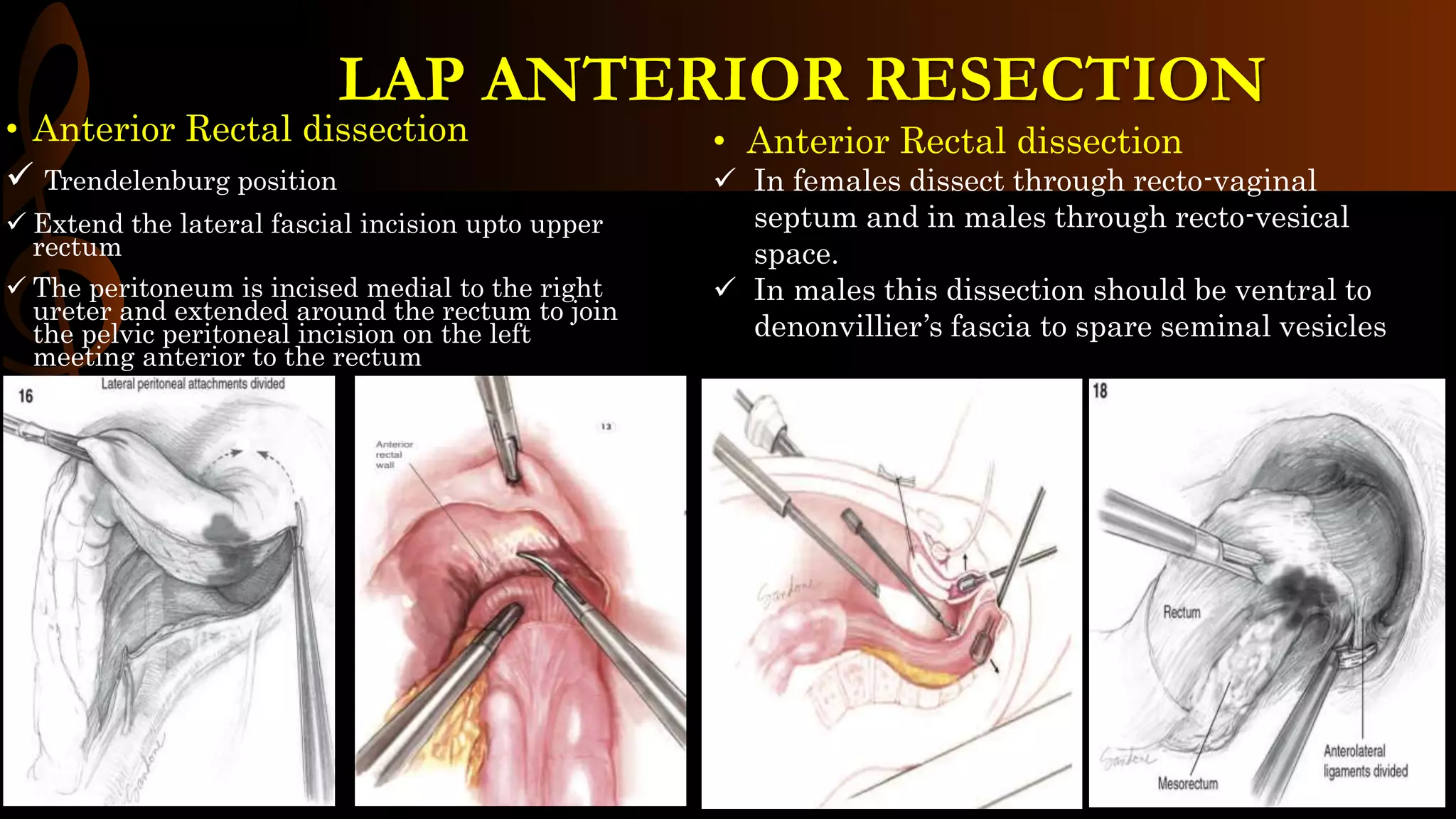
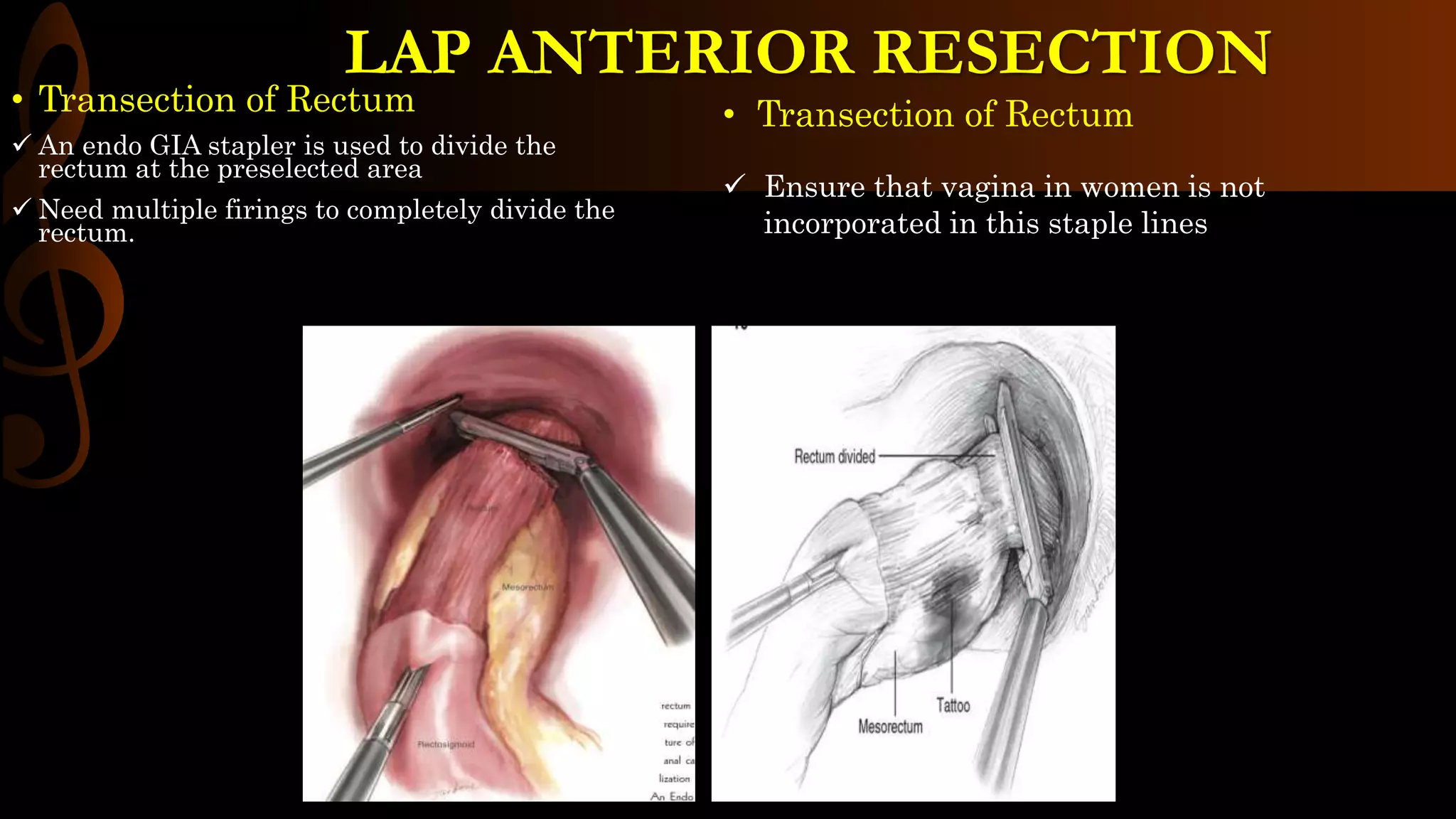
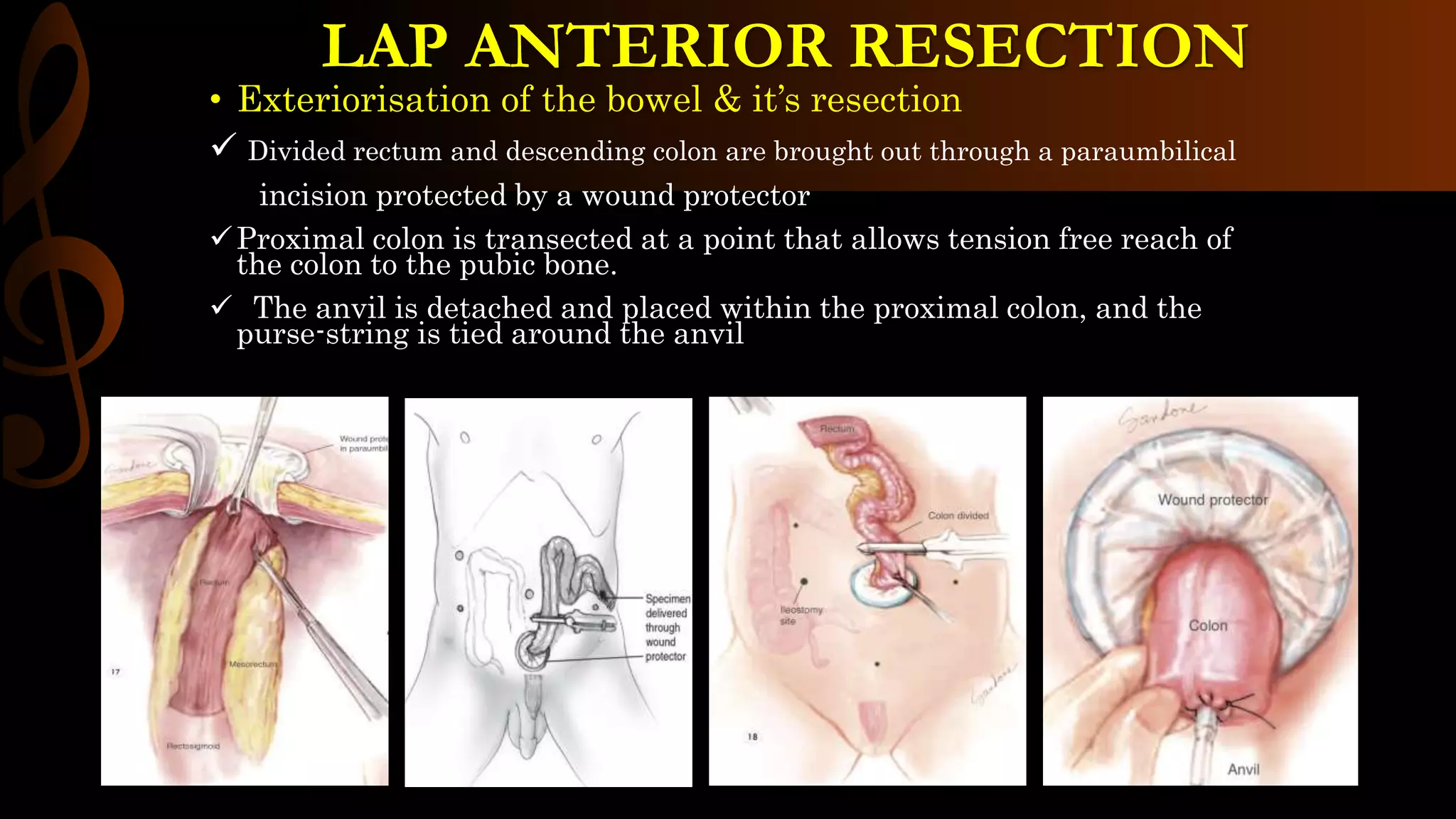
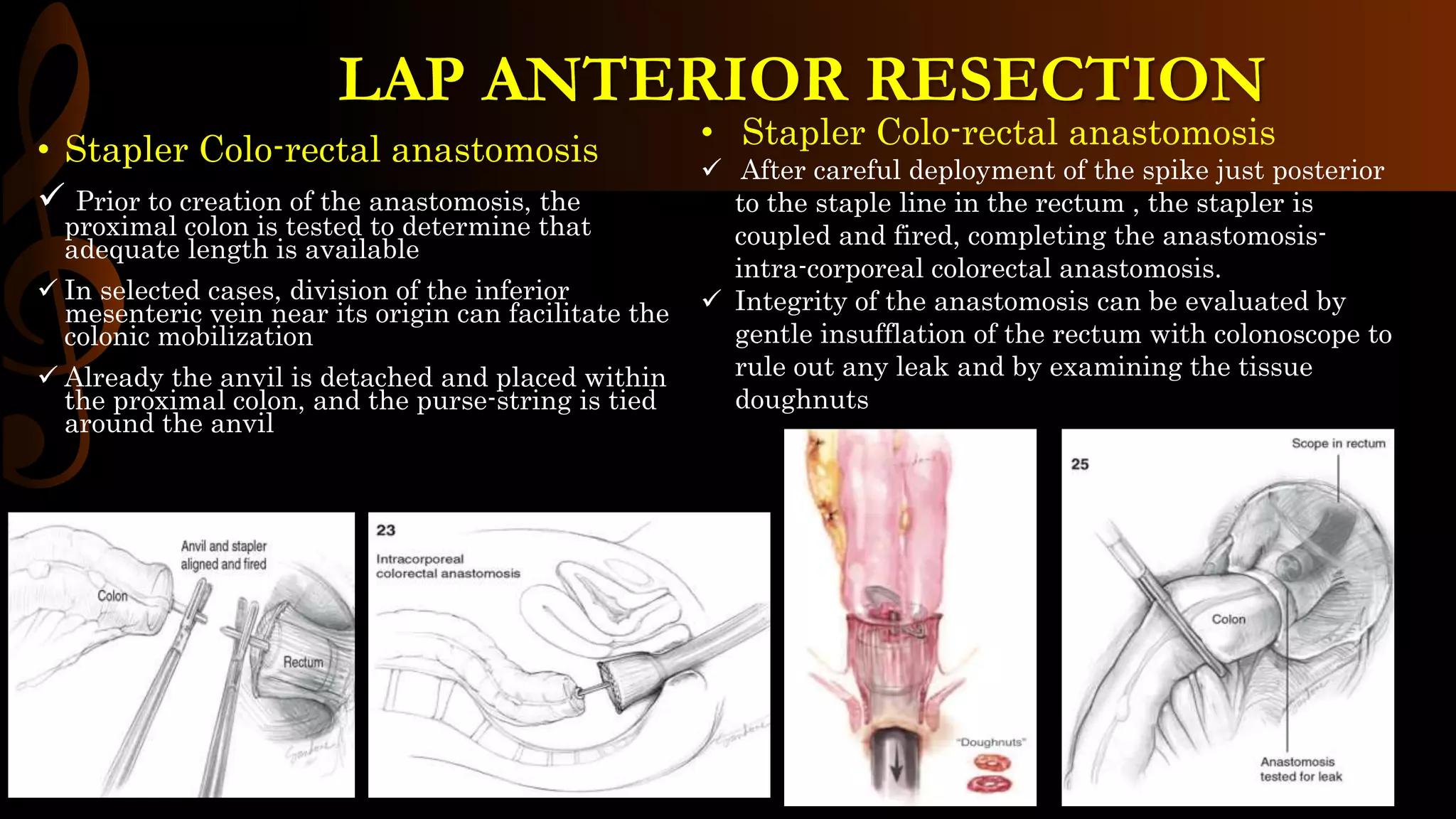
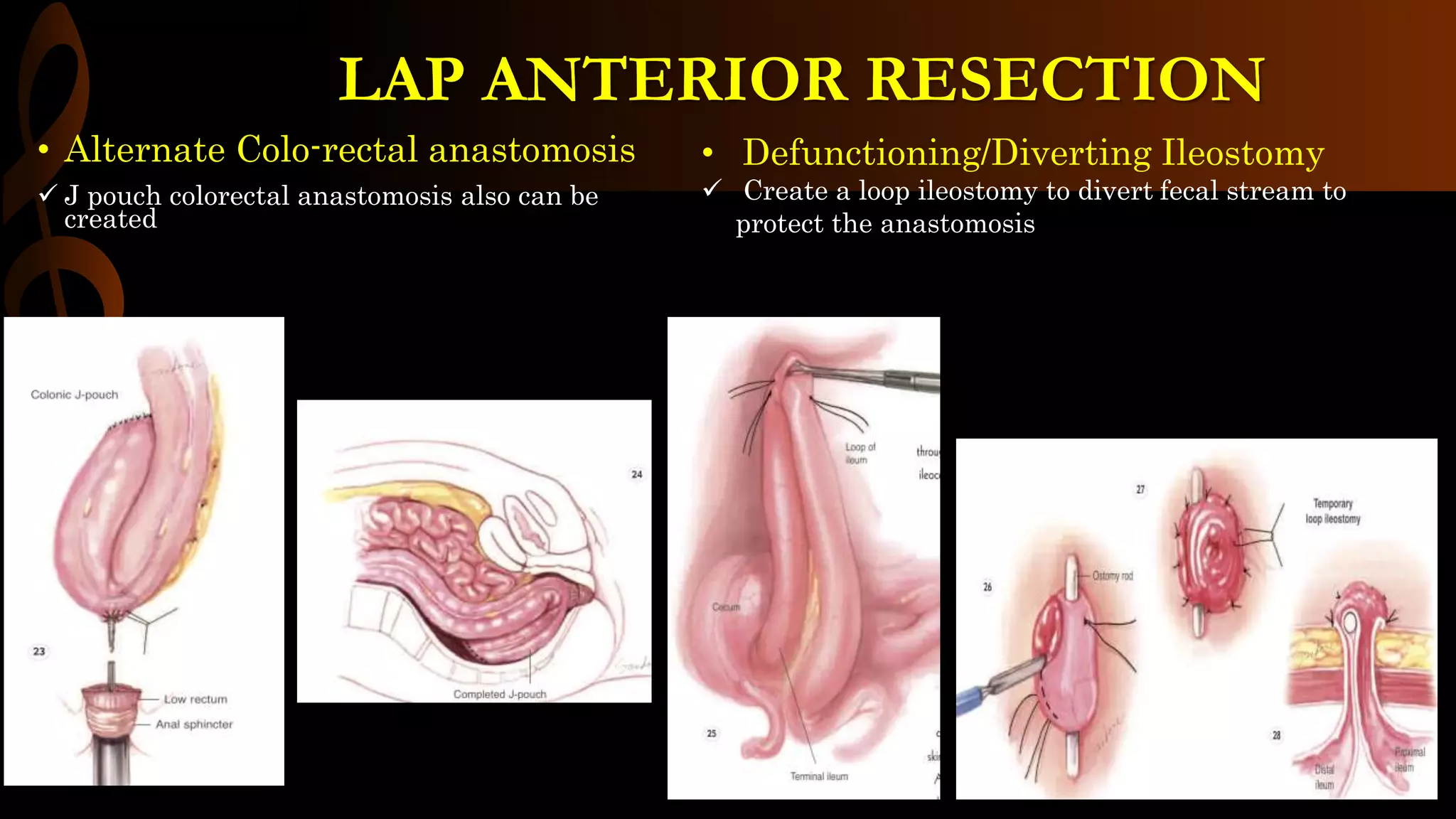
The document provides an overview of laparoscopic anterior resection surgery for rectal carcinoma, detailing its indications, contraindications, anesthesia, and positioning. It outlines the surgical procedure steps, including port placement, tumor mobilization, vascular ligation, excision, anastomosis, and post-operative care. Key considerations and potential complications are also highlighted to ensure successful outcomes and patient safety.