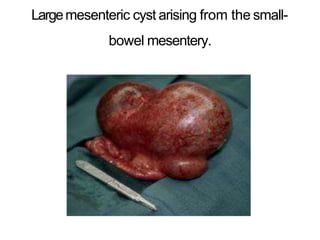
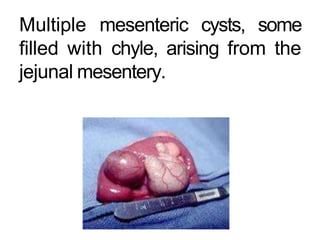
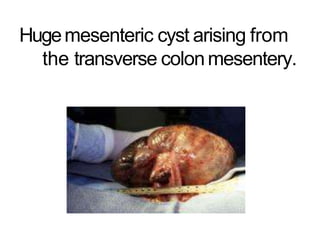
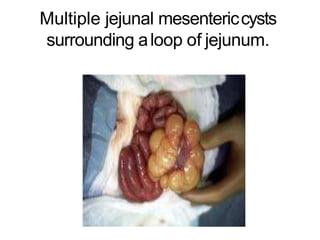
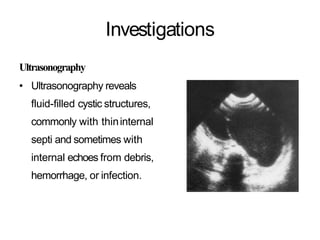
Mesenteric cysts are rare fluid-filled masses that form between the two layers of the small bowel mesentery. They have an incidence of 1 in 100,000 hospital admissions, with about 1/3 diagnosed in patients under 15 years old. The most common type is the chylolymphatic cyst, which occurs due to congenitally misplaced lymphatic tissue. Ultrasound and CT scans are used to identify the fluid-filled cystic structures. Surgical treatment involves enucleation of chylolymphatic cysts or excision with intestinal resection. Prognosis is generally favorable with low recurrence rates following complete excision.