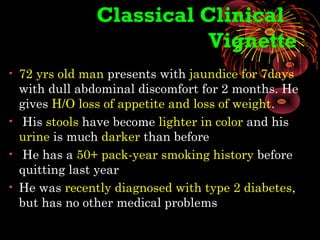
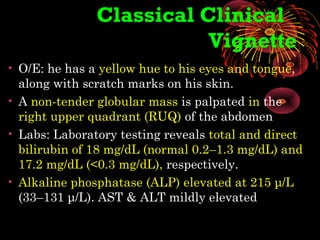
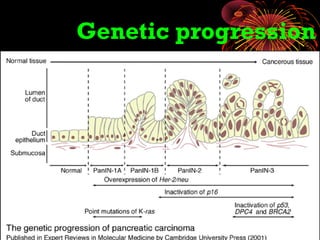
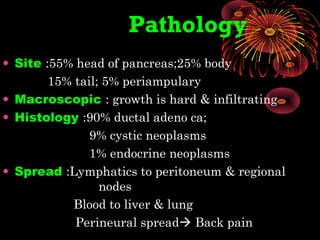
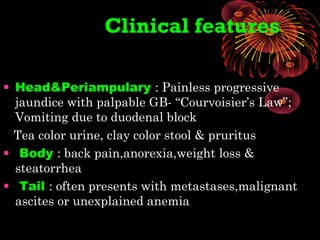
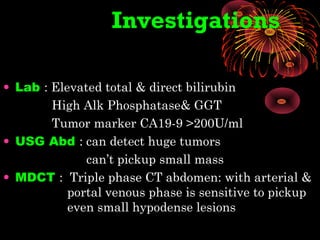
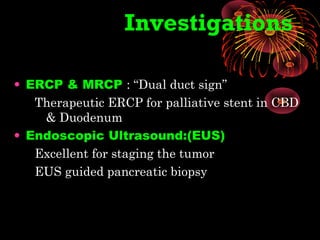
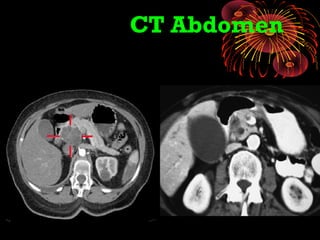
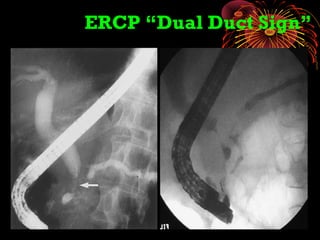
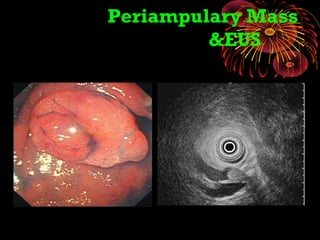
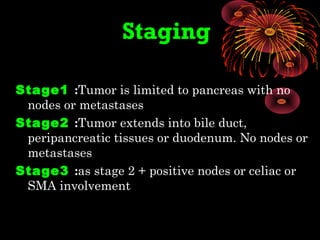
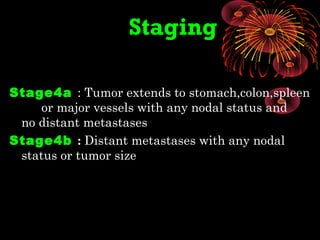
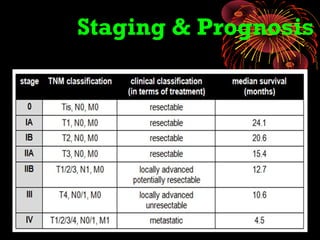
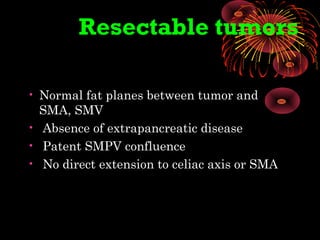
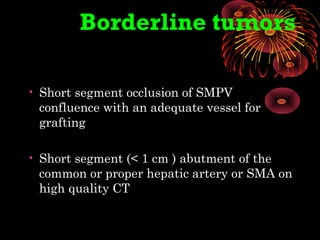
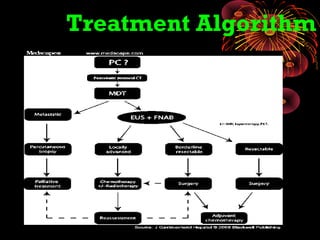
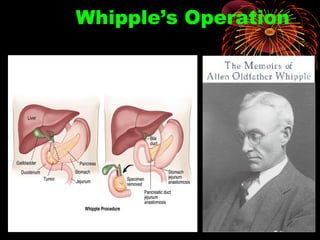
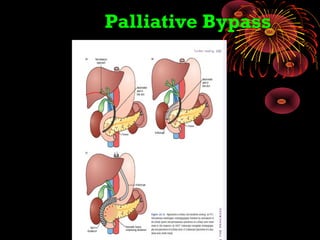
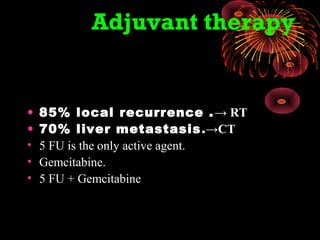
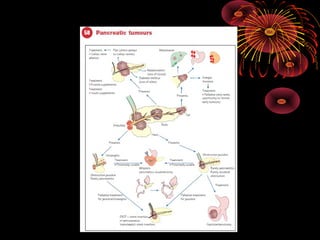
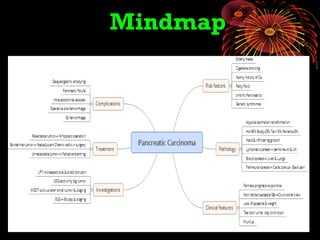
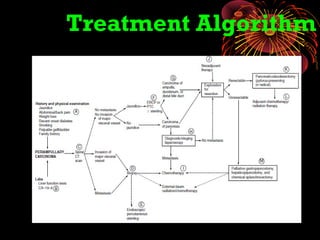
The document discusses pancreatic carcinoma, detailing a classical clinical vignette of a 72-year-old man presenting with jaundice, abdominal discomfort, and elevated bilirubin levels. It outlines the cancer's risk factors, pathology, clinical features, and current staging and treatment options, including surgical and palliative care methods. Additionally, it highlights the importance of early detection and the challenges of treatment due to the high recurrence and metastasis rates associated with this cancer.