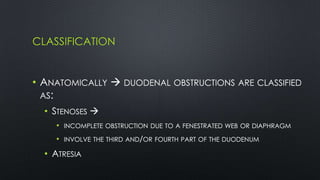
Duodenal atresia, occurring in 1 per 5000 to 10,000 live births, is a congenital condition characterized by varying degrees of gastrointestinal obstruction, with over 50% of cases associated with congenital anomalies such as trisomy 21. Diagnosis is often made via prenatal ultrasonography showing a 'double bubble' sign, and management includes careful pre-operative stabilization before surgical correction, which can be performed via open or laparoscopic techniques. Post-operative care focuses on monitoring feeding tolerance and managing potential complications, with risk stratification indicating varying mortality rates based on weight and associated anomalies.