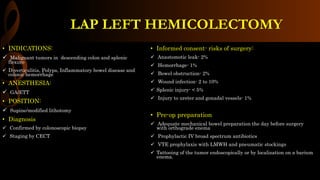
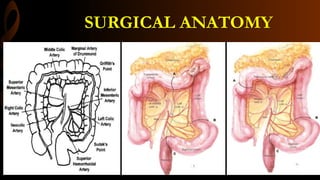
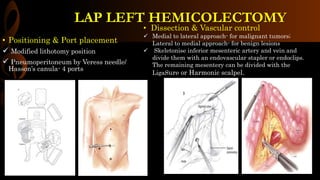
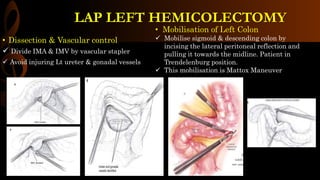
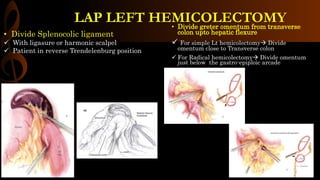
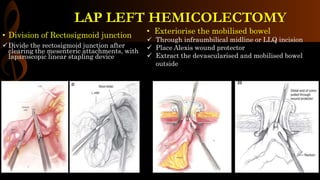
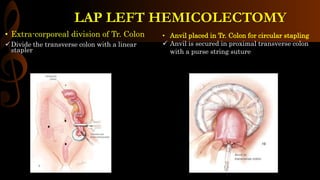
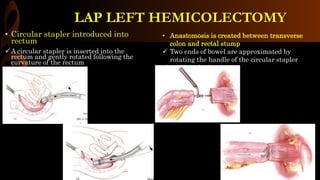
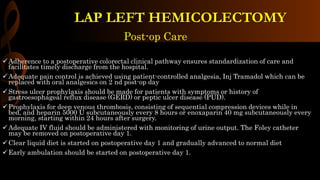
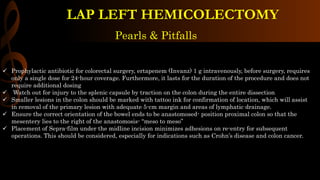
This document provides information on performing a laparoscopic left hemicolectomy surgery. Key steps include mobilizing the descending colon and sigmoid colon, dividing the inferior mesenteric artery and vein, dividing the splenic flexure and splenocolic ligament, and creating an intestinal anastomosis between the transverse colon and rectal stump using a circular stapler. Post-operative care involves pain management, thrombosis prophylaxis, early ambulation and diet advancement to ensure timely recovery.