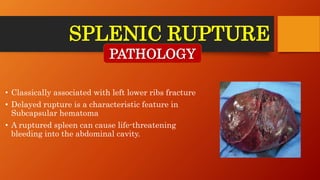
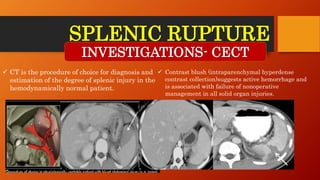
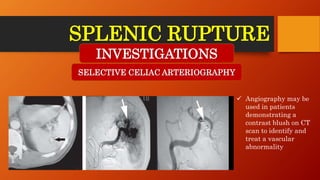
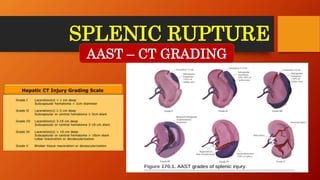
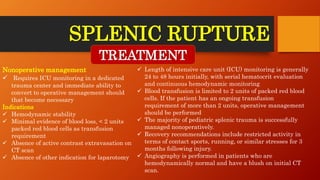
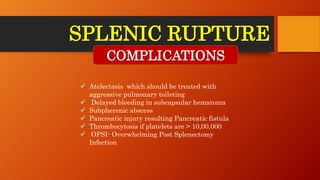
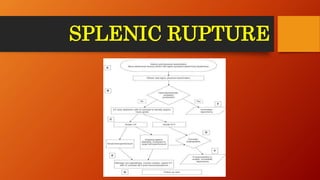
The document provides a comprehensive overview of splenic rupture caused by blunt or penetrating trauma, detailing its etiology, clinical features, diagnostic investigations, and treatment protocols. Nonoperative management is feasible for hemodynamically stable patients, while operative management is required for those in distress or failing conservative treatment. It also highlights potential complications such as overwhelming post-splenectomy infection (OPSI) and emphasizes the importance of vaccination prior to discharge.