1. Choledochal cysts are abnormal dilations of the bile ducts that are more common in Asia and women.
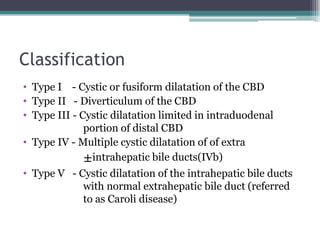
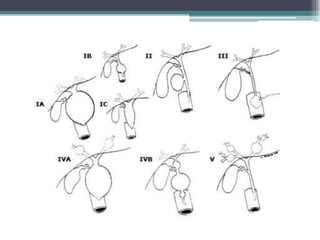
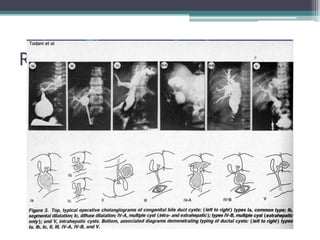
2. They are classified into 5 types based on location and extent of dilation.
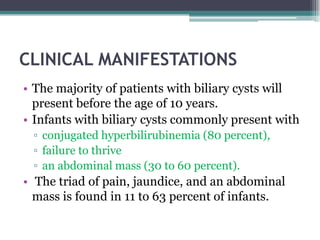
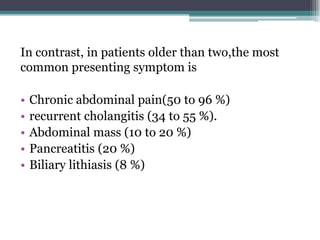
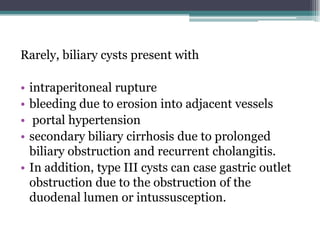
3. Presentation varies from jaundice and abdominal mass in children to pain and cholangitis in older patients.
4. Investigation involves ultrasound, CT, MRCP and cholangiography to determine type and rule out complications.
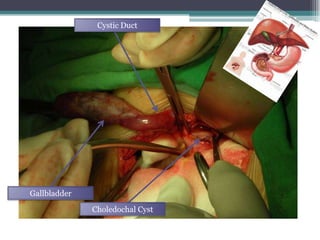
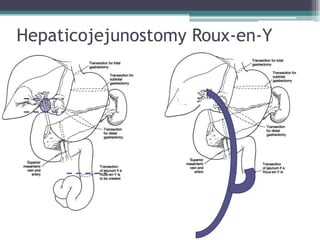
5. Treatment is complete excision of the cysts and biliary tree with Roux-en-Y hepaticojejunostomy, except for type III which can be managed endoscopically.
![Introduction
• Cyst dilatation thoughout the billiary tree
• Approximately 1 in 100,000 - 1 in 150,000
• More common in some asian countries(1:1000)
• More common in women (3-4 times)
• Frequently diagnosed in infancy or childhood
• Associated with billary cancer 10-30%[~16%]
(particularly cholangioCA-varies on age and type)](https://image.slidesharecdn.com/choledochalcyst-130428032225-phpapp01/85/Choledochal-cyst-2-320.jpg)
![Cholangiography
• Direct cholangiography (whether intraoperative,
percutaneous, or endoscopic) has a sensitivity of up to
100 percent for diagnosing biliary cysts and previously
was a commonly obtained test.
• can identify abnormal pancreatobiliary junction, and
filling defects due to stones or malignancy.
• Increase risk of cholangitis and pancreatitis. [
Patients with cystic disease are greater risk for these
complications ]](https://image.slidesharecdn.com/choledochalcyst-130428032225-phpapp01/85/Choledochal-cyst-26-320.jpg)
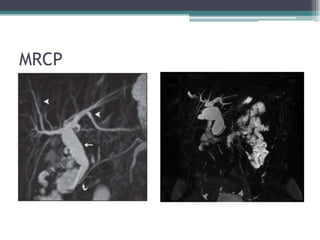
![Magnetic resonance
cholangiopancreatography [MRCP]
• Does not have the risks of cholangitis and
pancreatitis as direct cholangiography
• Sensitivity 73 - 100 %.
• less sensitive than direct cholangiography for
excluding obstruction.
• The data are variable with regard to its ability to
diagnose an abnormal pancreatobiliary junction.
[46-75%]](https://image.slidesharecdn.com/choledochalcyst-130428032225-phpapp01/85/Choledochal-cyst-28-320.jpg)