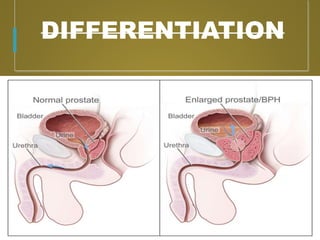
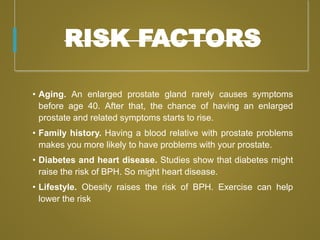
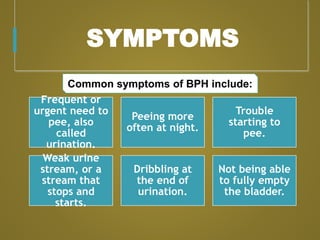
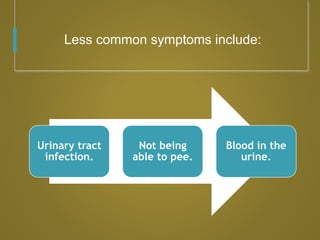
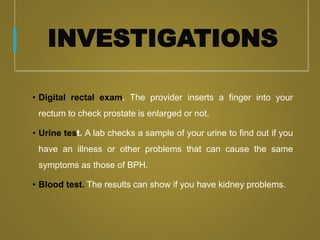
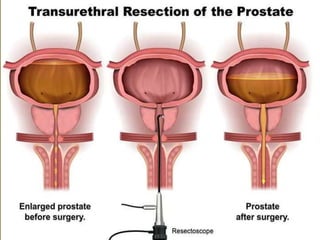
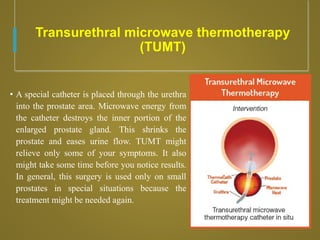
Benign prostatic hyperplasia (BPH) is an age-related condition characterized by prostate enlargement, leading to urinary problems such as frequent urination, difficulty starting to urinate, and incomplete bladder emptying. Diagnosis involves exams like digital rectal exams and urine tests, while treatment options range from medications and lifestyle changes to various surgical procedures. Complications of BPH include urinary retention, infections, and potential kidney damage, making early intervention important.