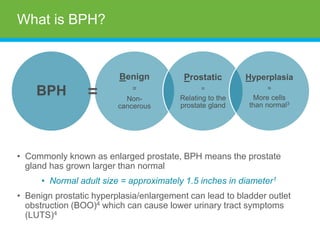
This document provides an overview of benign prostatic hyperplasia (BPH) for a physician to present to patients. It defines what the prostate is and how BPH affects it. Symptoms, diagnosis, and various treatment options are described, including watchful waiting, medications, minimally invasive therapies like TUMT and laser, and invasive surgeries. Insurance coverage considerations are also mentioned. The physician is advised to consult with patients' urologists to determine the best individual treatment plan.


![[Physician Name]
• [Credentials/Specialty/Title]
• [Practice Name/Hospital]
‒ [Locations]
‒ [Contact Information]
• [Education]
• [Affiliations]](https://image.slidesharecdn.com/amsusbph-009772b-bph-ppt-060314-unbranded-final-for-hcp-21-221116083020-416625a9/85/BPH-3-320.jpg)
![[Physician]
• Specializes in
‒ [Include additional information about your practice]](https://image.slidesharecdn.com/amsusbph-009772b-bph-ppt-060314-unbranded-final-for-hcp-21-221116083020-416625a9/85/BPH-4-320.jpg)