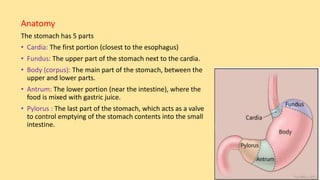
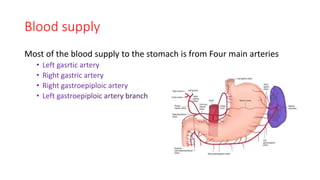
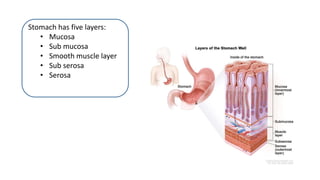
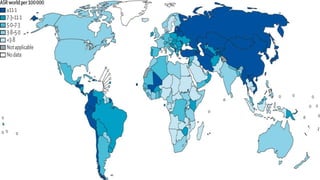
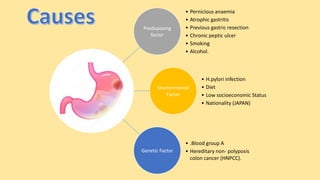
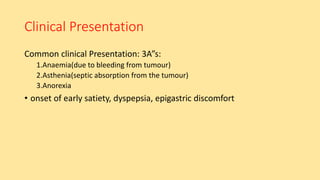
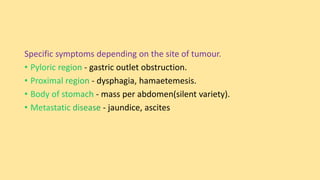
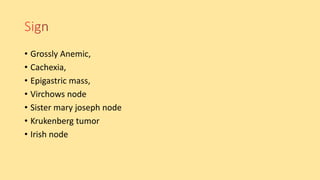
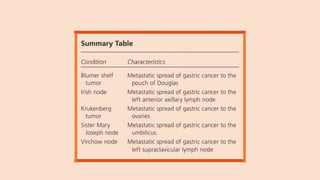
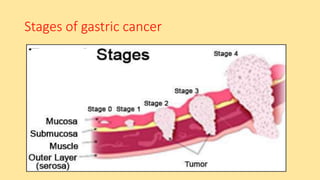
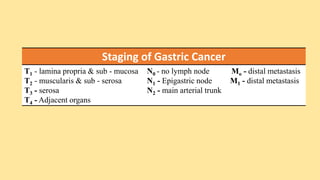
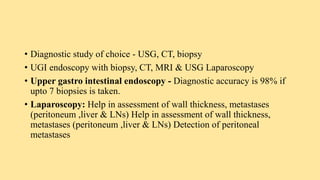
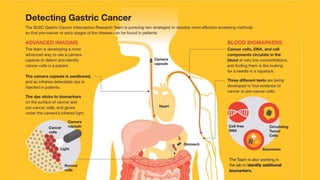
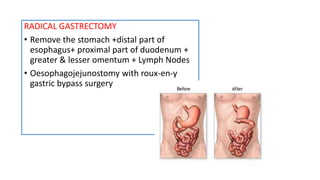
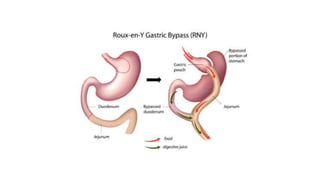
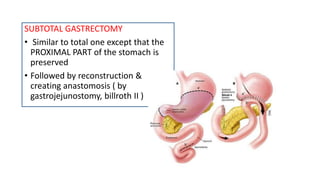
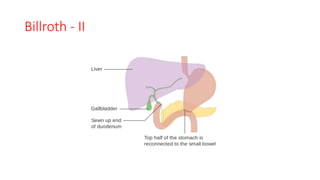
This document provides information about the anatomy, blood supply, drainage, layers and cancer of the stomach. It describes the five parts of the stomach and their functions. It also discusses the predisposing factors, clinical presentation, investigations, staging, spread, management including surgery, chemotherapy and radiotherapy, postoperative orders and complications of gastric cancer. Nursing diagnoses and management of a patient post-gastrectomy are also outlined.