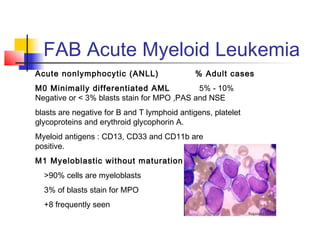
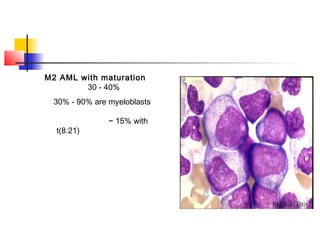
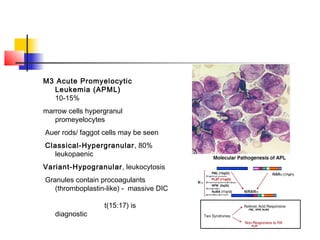
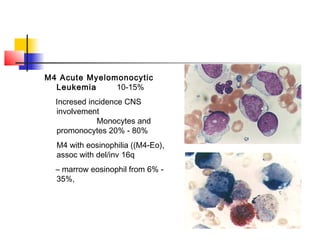
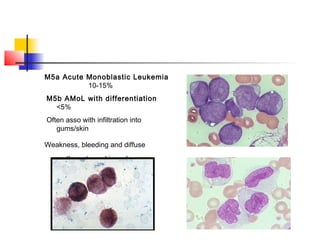
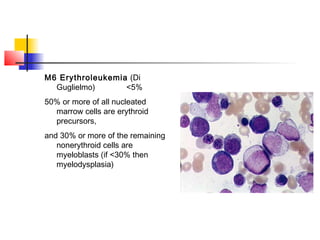
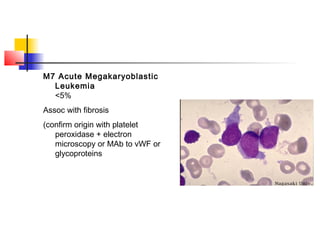
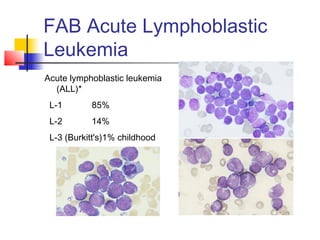
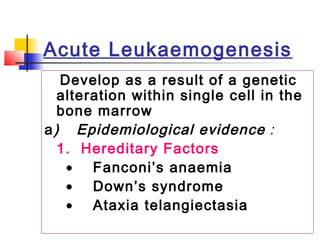
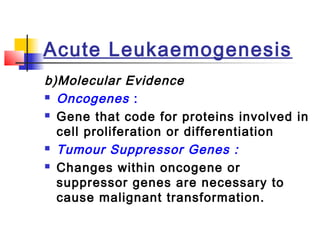
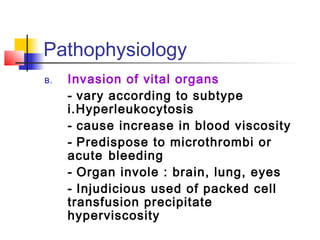
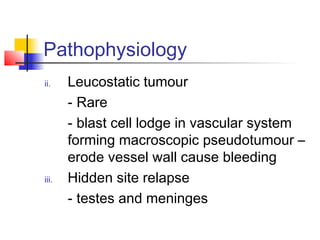
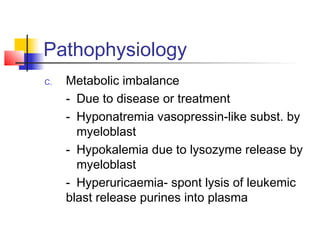
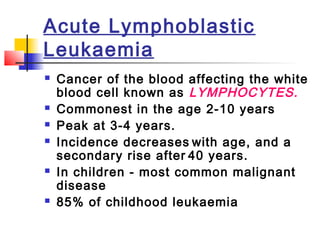
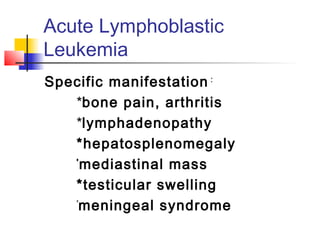
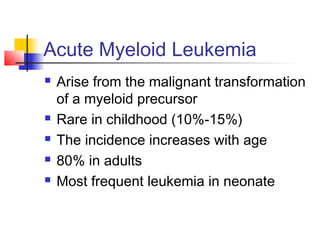
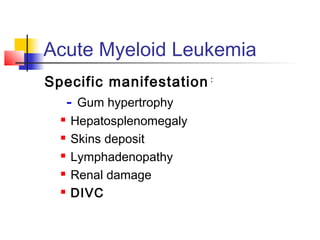
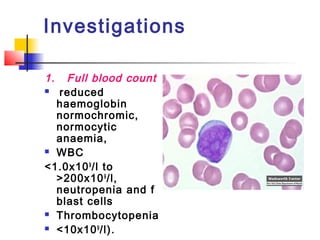
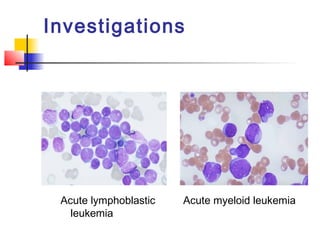
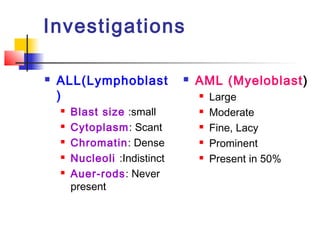
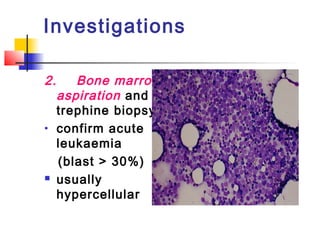
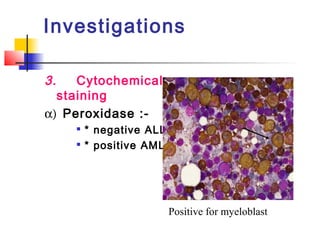
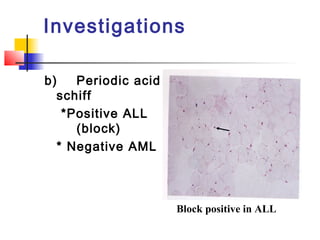
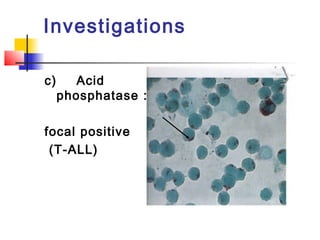
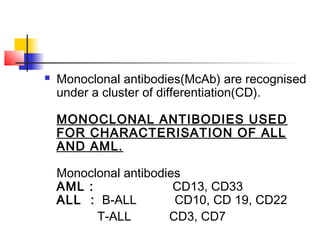
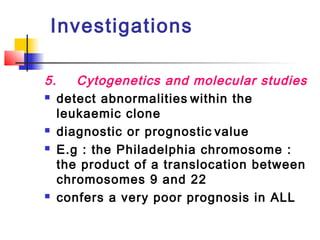
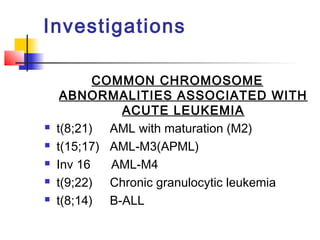
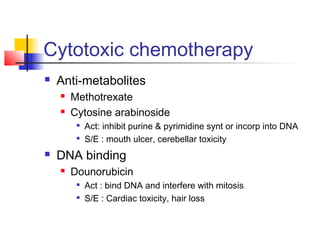
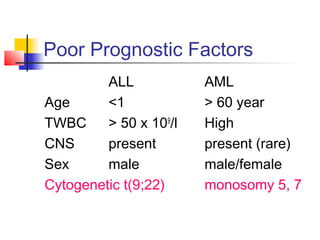
The document provides a comprehensive overview of acute leukemia, outlining its definition, classification, pathogenesis, and diagnostic requirements. It details the two main types, Acute Lymphoblastic Leukemia (ALL) and Acute Myeloid Leukemia (AML), along with their respective characteristics, complications, and management strategies. Additionally, the document discusses laboratory investigations necessary for diagnosis and the prognostic factors influencing treatment outcomes.