This document provides guidelines for the evaluation and management of pediatric community-acquired pneumonia (PCAP). It defines pneumonia and discusses the etiology, pathogenesis, clinical manifestations, diagnostic criteria, and treatment recommendations for different classifications of PCAP cases. Empiric antibiotic therapy and monitoring response to treatment are also addressed. The document aims to outline best practices for diagnosing and managing PCAP based on classification of the case.
















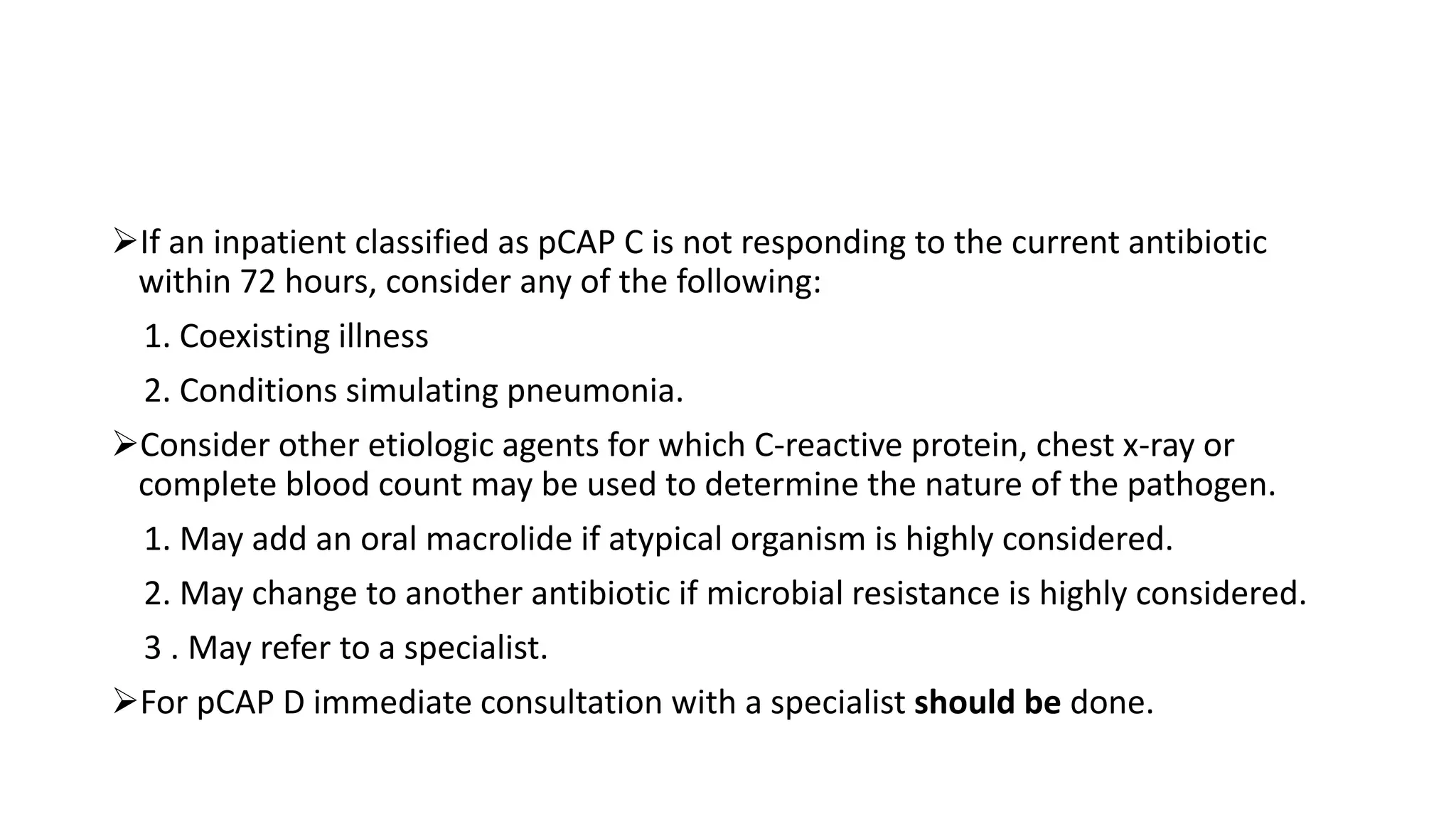
![1. For a patient who has been classified as pCAP A or B without previous antibiotic,
A. Amoxicillin [40-50 mg/kg/day, maximum dose of 1500 mg/day in 3 divided doses
for at most 7 days] is the drug of choice.
Amoxicillin may be given for a minimum of 3 days .
Amoxicillin may be given in 2 divided doses for a minimum of 5 days.
B. Azithromycin [10 mg/kg/day OD for 3 days or 10mg/kg/day at day 1 then
5mg/kg/day for days 2 to 5 maximum dose of 500mg/day], .
C.Clarithromycin [15 mg/kg/day, maximum dose of 1000 mg/day in 2 divided doses
for 7 days] given to those patients with known hypersensitivity to amoxicillin.](https://image.slidesharecdn.com/pediatriccommunity-170920120845/75/Pediatric-community-Acquired-Pneumonia-24-2048.jpg)
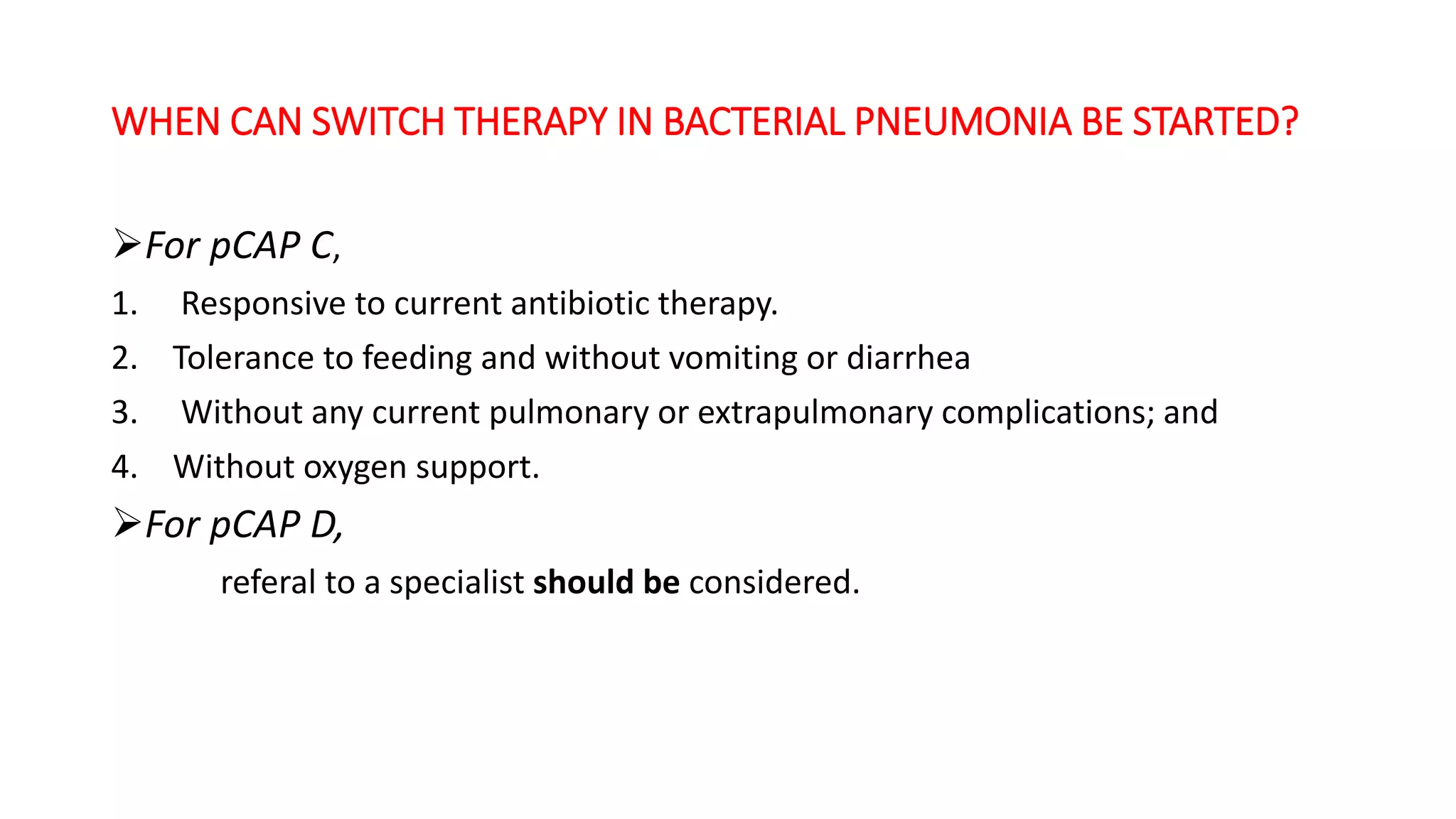
![2. For a patient who has been classified as pCAP C, without previous antibiotic,
Requiring hospitalization
A .Has completed the primary immunization against H. influenza type b,penicillin
G [100,000 units/kg/day in 4 divided doses] administered as monotherapy is the
drug of choice.
B. Has not completed the primary immunization or immunization status
unknown against H. influenza type b, ampicillin [100 mg/kg/day in 4 divided doses]
administered as monotherapy is the drug of choice.](https://image.slidesharecdn.com/pediatriccommunity-170920120845/75/Pediatric-community-Acquired-Pneumonia-25-2048.jpg)
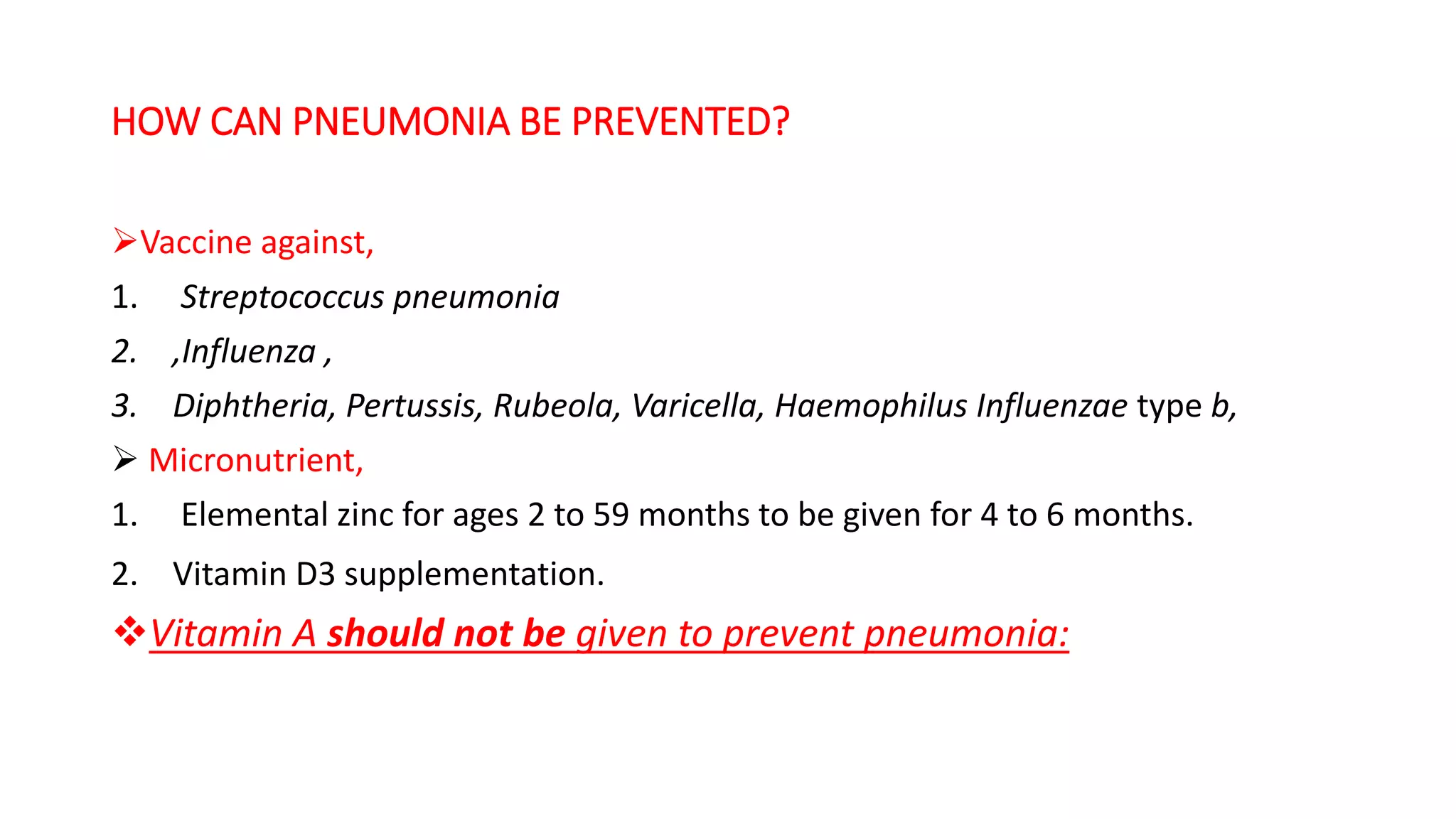
![Above15 years of age ,
• A parenteral non-antipseudomonal β-lactam (β-lactam/(BLIC), cephalosporin or
carbapenem] + extended macrolide, or a parenteralnon-antipseudomonal β-
lactam [β-lactam/ BLIC],cephalosporin or carbapenem + respiratory
Fluoroquinolone administered as combination therapy may be given.
• and who can tolerate oral feeding and does not require oxygen support,
amoxicillin [40-50 mg/kg/day, maximum dose of 1500 mg/day in 3 divided doses
for at most 7 days] may be given on an outpatient basis.](https://image.slidesharecdn.com/pediatriccommunity-170920120845/75/Pediatric-community-Acquired-Pneumonia-26-2048.jpg)