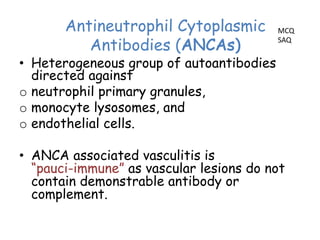
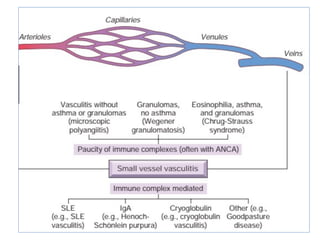
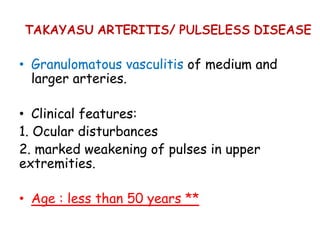
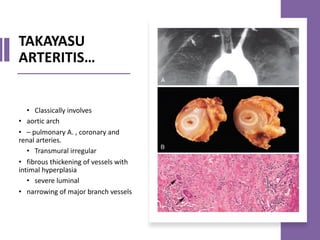
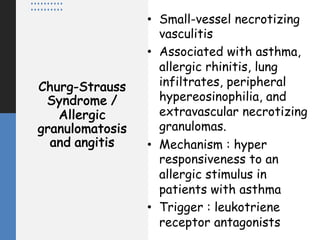
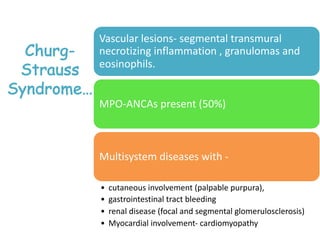
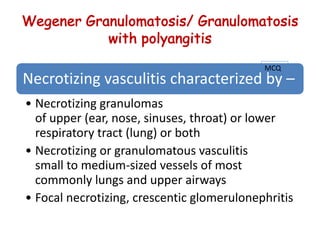
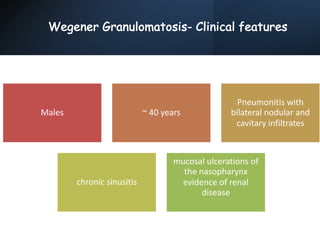
The document outlines the objectives and classifications of vasculitis, describing its causes, pathogenesis, and clinical presentations across various types. Key forms discussed include giant-cell arteritis, Takayasu arteritis, polyarteritis nodosa, Kawasaki disease, and others, each with distinct morphological and clinical features. The document emphasizes the role of immune responses, specific autoantibodies, and infections in the pathology of vasculitis, highlighting the need for prompt recognition and treatment to prevent serious complications.