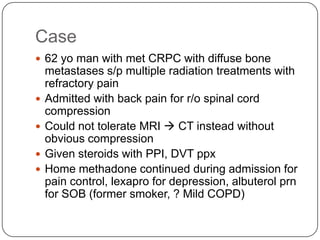
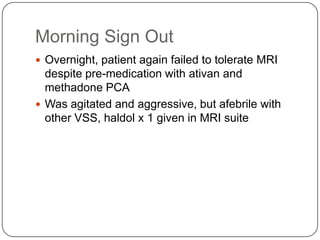
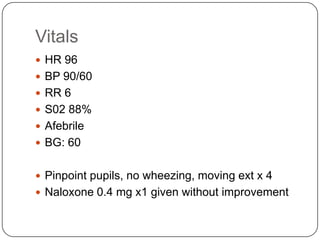
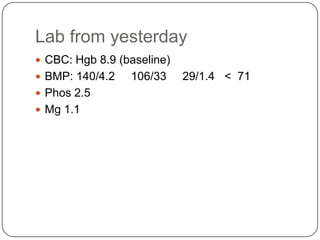
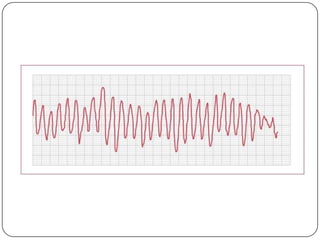
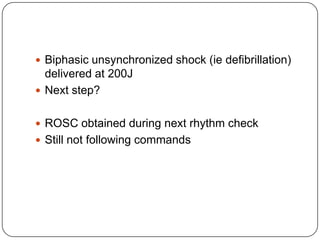
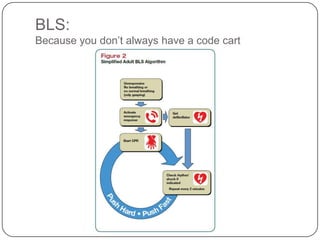
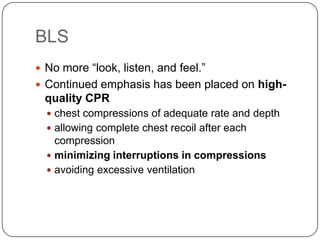
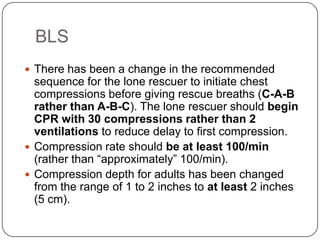
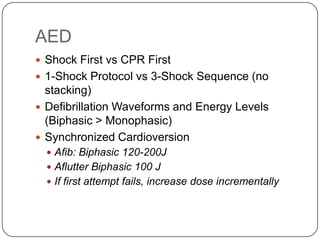
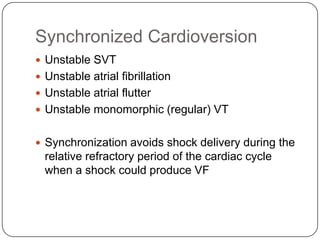
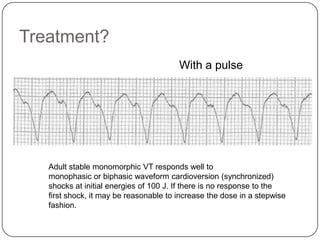
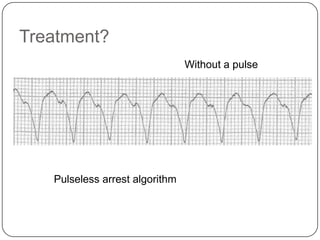
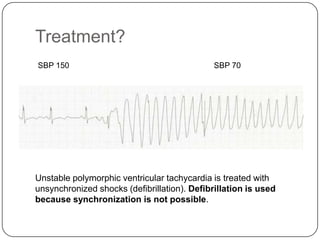
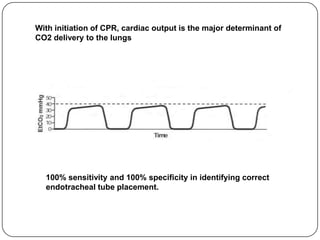
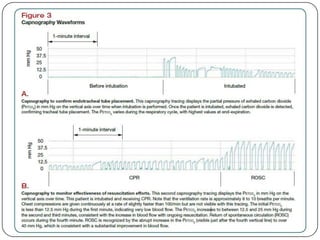
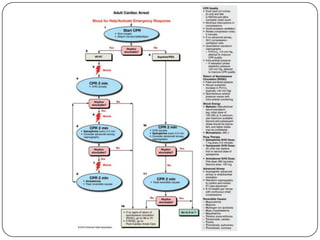
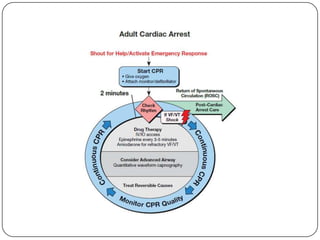
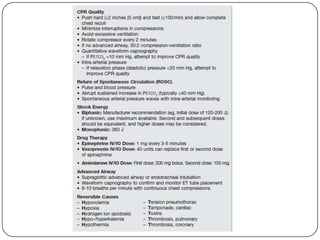
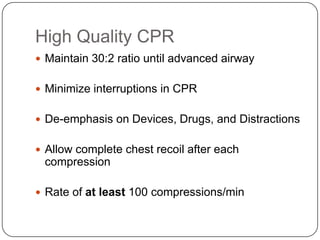
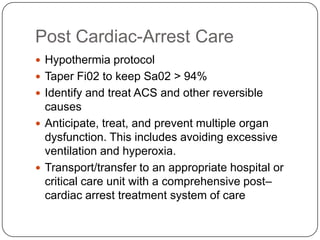
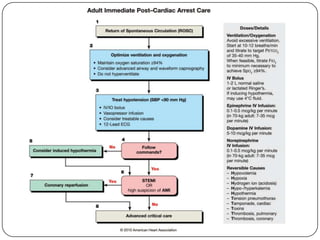
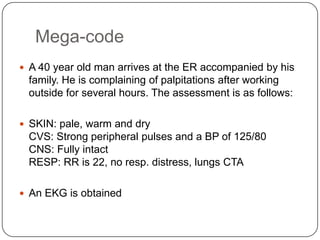
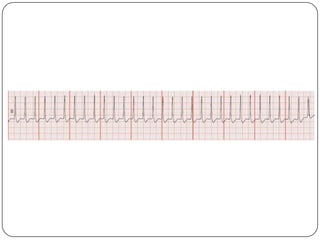
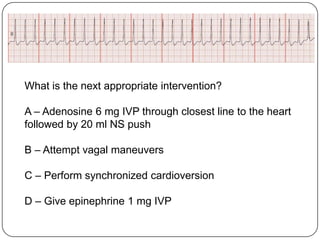
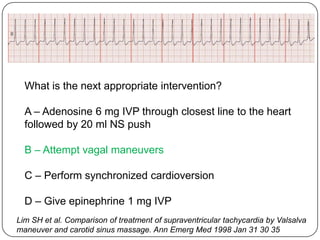
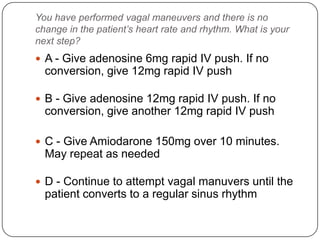
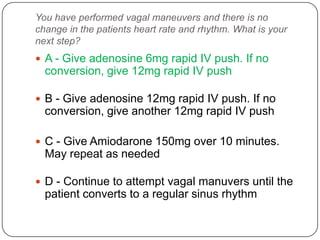
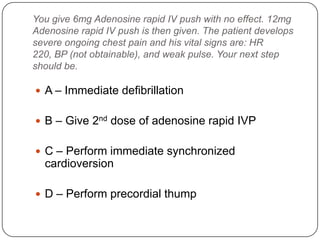
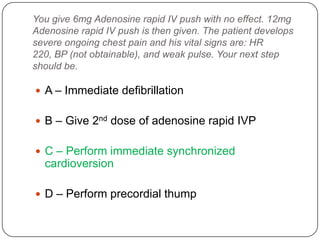
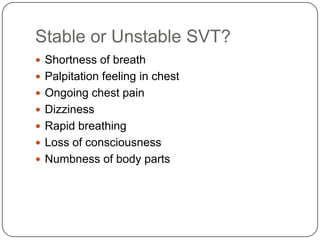
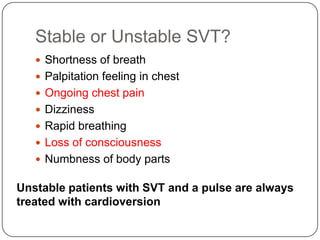
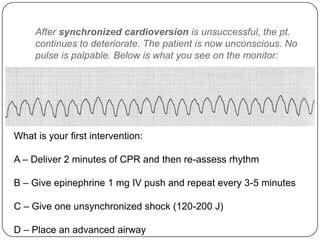
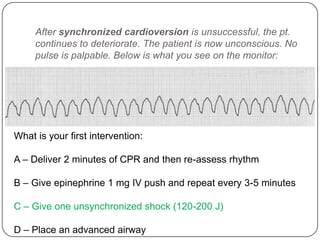
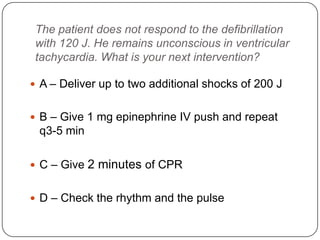
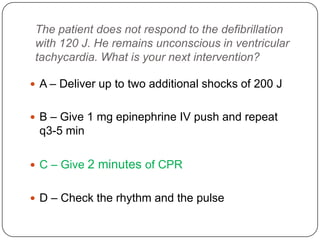
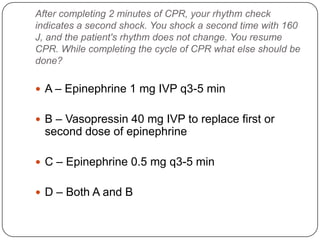
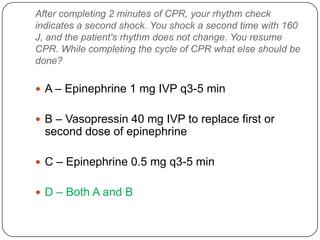
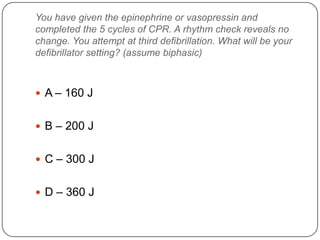
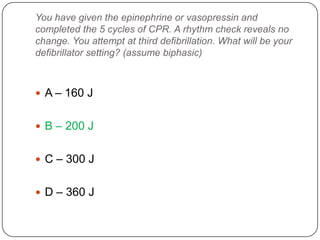
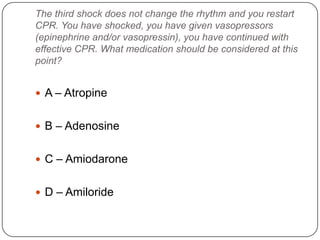
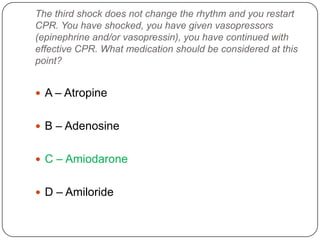
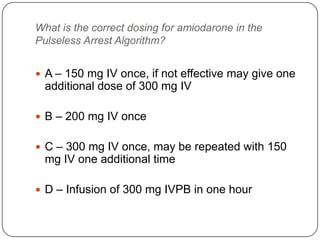
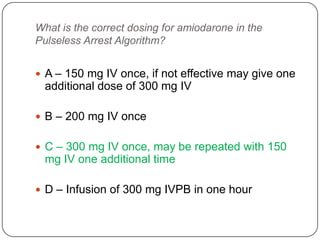
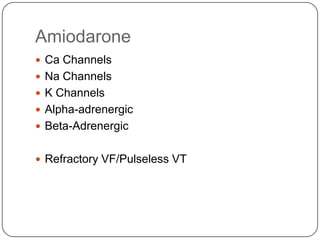
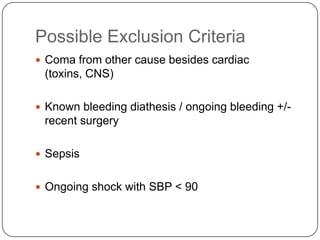
This document summarizes an ACLS update and review presentation. It describes a case of a 62-year-old man admitted with back pain who became unresponsive after being given Haldol. His vitals showed bradycardia and hypotension. He received biphasic shocks and regained a pulse but did not follow commands. The presentation reviewed changes to BLS protocols, including performing chest compressions before breaths for lone rescuers and a compression rate of at least 100/min. It also discussed treatment for pulseless arrest, synchronized cardioversion, and amiodarone dosing. The importance of therapeutic hypothermia for unresponsive post-cardiac arrest patients was emphasized.