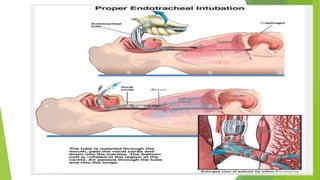
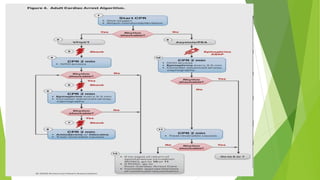
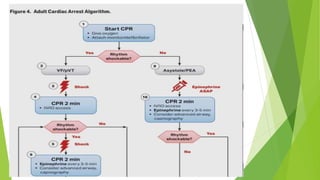
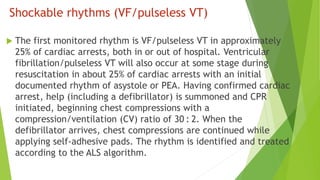
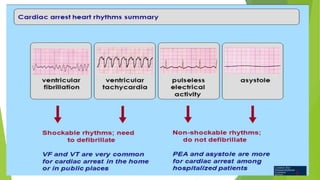
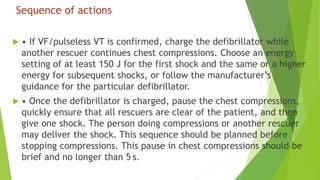
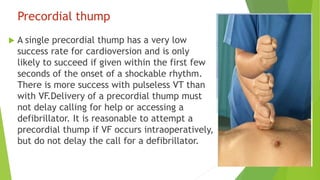
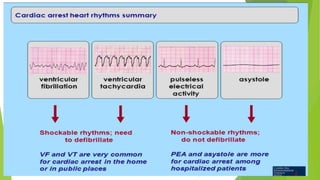
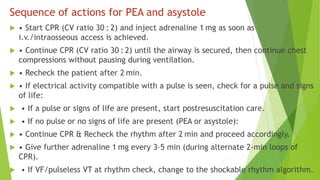
The document provides an overview of the 2020 American Heart Association guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care, emphasizing the critical response needed for cardiac arrest. It details best practices for high-quality chest compressions, the management of shockable and non-shockable rhythms, and the importance of timely defibrillation, as well as the need to address reversible causes of cardiac arrest. Effective CPR techniques and collaborative emergency response are highlighted to maximize survival chances and minimize neurological damage.
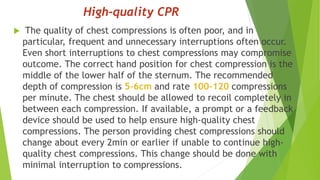
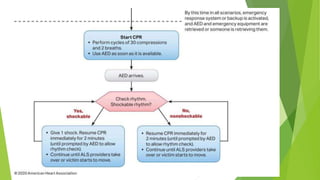

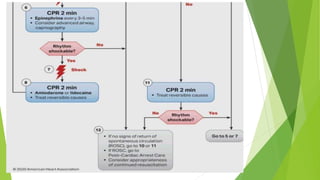
![CPR Quality
Push hard (at least 2 inches [5 cm]) and fast (100-120/min)
and allow complete chest recoil.
Minimize interruptions in compressions.
Avoid excessive ventilation.
Change compressor every 2 minutes, or sooner if fatigued.
If no advanced airway, 30:2 compression-ventilation ratio.
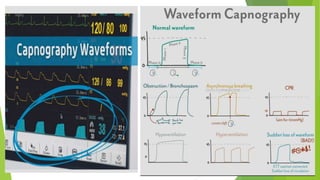
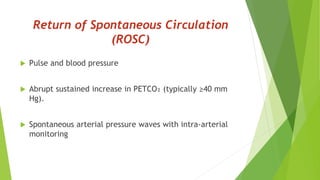
Quantitative waveform capnography
-If PETCO₂ is low or decreasing, reassess CPR quality.](https://image.slidesharecdn.com/cpr-240503153225-7d47212a/85/CPR-introduction-and-mechanisms-to-do-pptx-27-320.jpg)