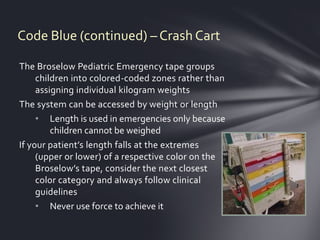
The document outlines protocols for responding to cardiopulmonary arrests, known as Code Blues. It describes initiating Basic Life Support, Advanced Cardiac Life Support, or Pediatric Advanced Life Support depending on the patient. It provides details on activating emergency codes, assembling code teams, performing immediate interventions like CPR and defibrillation, notifying physicians, and transferring patients to the emergency department. Crash carts and equipment are also discussed, including obtaining replacement carts and charging used items.