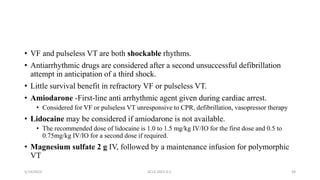
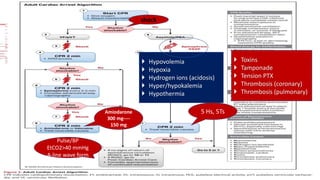
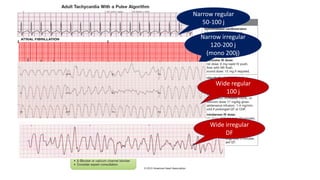
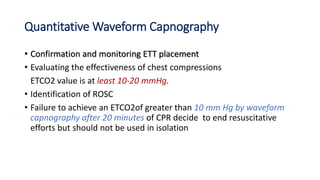
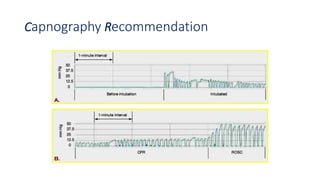
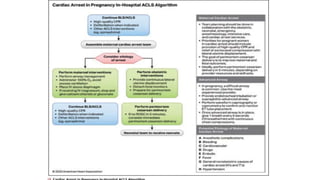
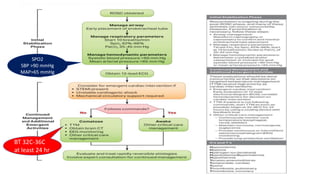
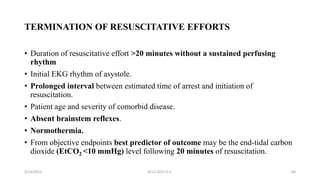
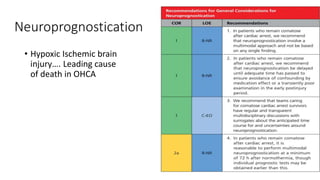
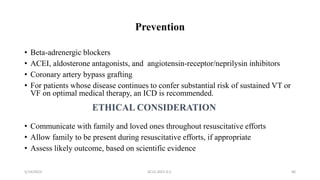
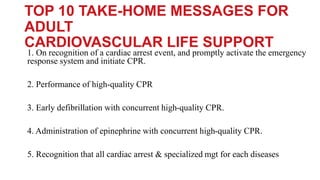
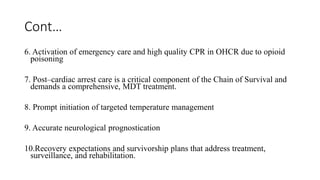
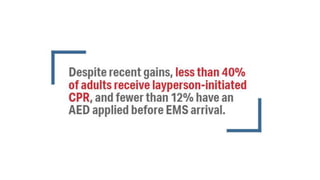
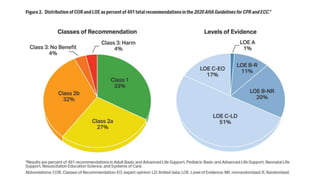
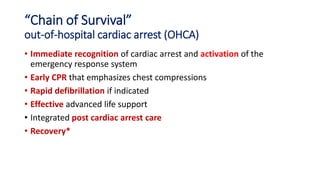
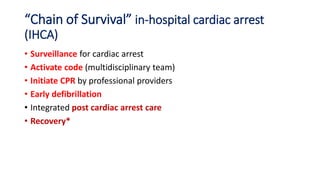
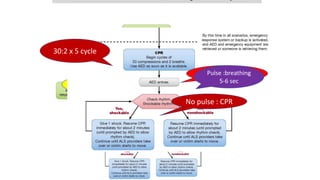
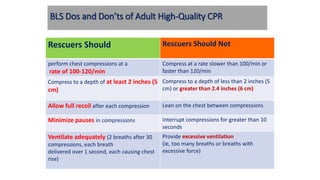
The document outlines advanced cardiovascular life support (ACLS) techniques, covering topics such as basic life support (BLS), the chains of survival for out-of-hospital and in-hospital cardiac arrests, and the importance of immediate CPR and defibrillation. It details specific procedures for responding to cardiac arrest, including the use of automated external defibrillators, and the administration of medications like epinephrine and amiodarone during resuscitation efforts. The document also emphasizes the significance of post-cardiac arrest care and neuroprognostication in improving survival and recovery outcomes.






















![Defibrillator
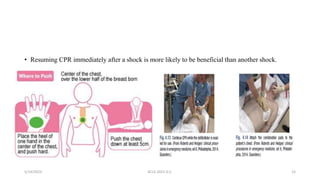
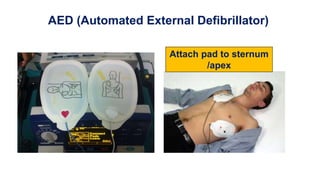
1. Right of the upper sternum below the clavicle
2. left 5th IC space ant. Axillary's line.
• Technique:
1. Apply pressure to the paddle [10kg] to decrease thoracic
impedance (the distance by pr. The fat).
2. keep the defibrillator paddles at least 12.5 cm from the
pace maker if there is.
3. Keep oxygen flow away from paddle and area of the
patient’s bed ; and place them at least 3.5 to 4 feet away from
the patient’s chest.
4. Don’t remove the paddle until 3 DC shock performed.](https://image.slidesharecdn.com/advancedcardiovascularlifesupportacls-230514105823-3707ca88/85/Advanced-Cardiovascular-Life-Support-ACLS-pptx-45-320.jpg)