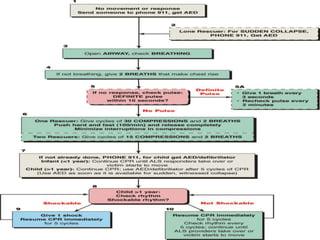
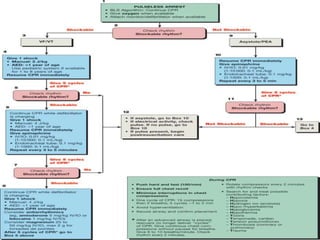
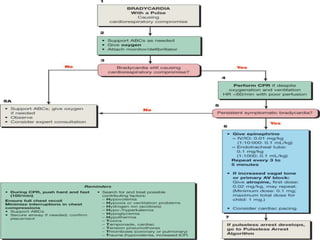
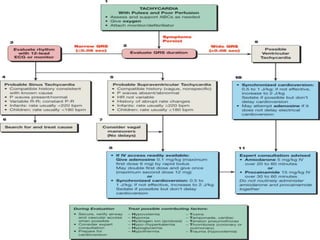
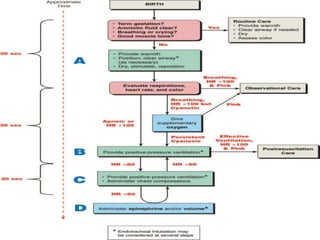
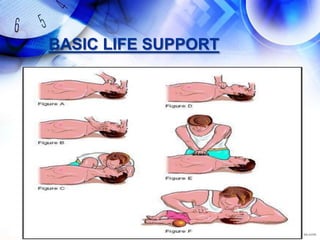
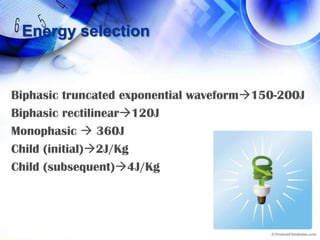
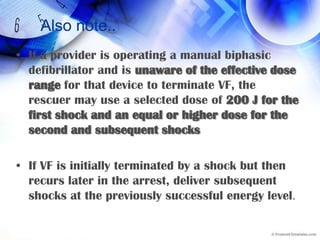
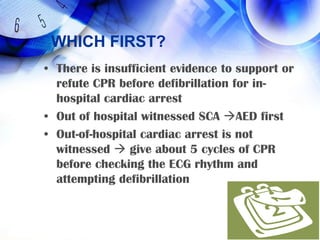
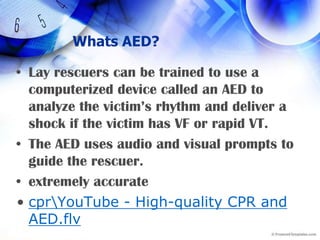
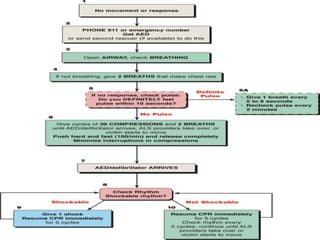
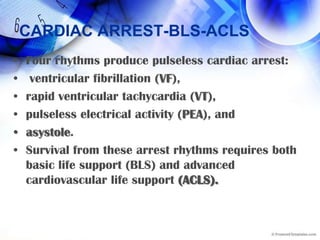
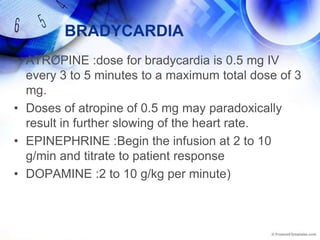
This document provides a summary of basic life support (BLS) and advanced cardiovascular life support (ACLS) protocols for treating cardiac arrest. It outlines the key steps in BLS including checking for response, activating emergency services, providing rescue breathing and chest compressions. It emphasizes the importance of high-quality chest compressions during CPR. The document also summarizes ACLS protocols for defibrillation, cardioversion, management of various cardiac rhythms like ventricular fibrillation and asystole, and administering appropriate drug therapies.


![Later…..When an advanced airway is in place [ETT/LMA/COMBITUBE]the compressing rescuer should give continuous chest compressions at a rate of 100 per minute without pauses for ventilation. The rescuer delivering ventilation provides 8 to10 breaths per minute.](https://image.slidesharecdn.com/blsandacls-091008142409-phpapp02/85/CPR-GUIDELINES-2005-15-320.jpg)
![PUSH HARD AND FASTFAST100 compressions per minute, HARD with a compression depth of 11⁄2 to 2 inches (approximately 4 to 5 cm). Allow the chest to recoil completely after each compression, and allow approximately equal compression and relaxation timesMinimize interruptions[Ideally, compression should be interrupted only for ventilation (until an advanced airway is placed), rhythm check, or shock delivery].](https://image.slidesharecdn.com/blsandacls-091008142409-phpapp02/85/CPR-GUIDELINES-2005-16-320.jpg)

![VF/VTDRUGSIf VF/VT persists after delivery of 1 or 2 shocks plus CPR, give a vasopressor (epinephrine every 3 to 5 minutes during cardiac arrest; one dose of vasopressinmay replace either the first or second dose of epinephrineWhen VF/pulseless VT persists after 2 to 3 shocks plus CPR and administration of a vasopressor, consider administering an antiarrhythmic such as amiodarone[ if unavailablelignocaine]magnesium for torsades de pointes associated with a long QT interval](https://image.slidesharecdn.com/blsandacls-091008142409-phpapp02/85/CPR-GUIDELINES-2005-37-320.jpg)
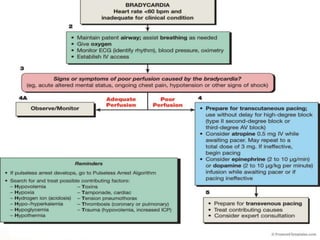
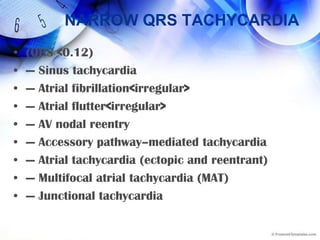
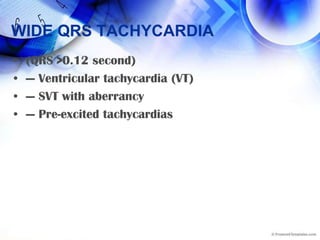
![Approach….Rate-related cardiovascular compromise[altered mental status, ongoing chest pain, hypotension], provide immediate synchronized cardioversionstable 12-lead ECG and evaluate the rhythm determine treatment options/may await expert consultation [because treatment has the potential for harm].](https://image.slidesharecdn.com/blsandacls-091008142409-phpapp02/85/CPR-GUIDELINES-2005-48-320.jpg)