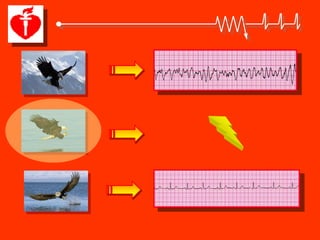
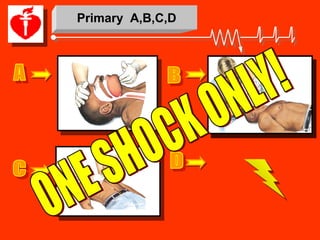
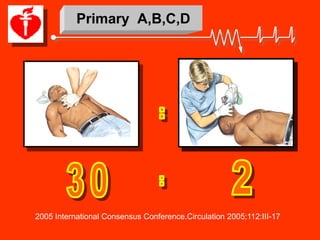
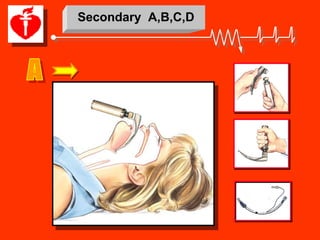
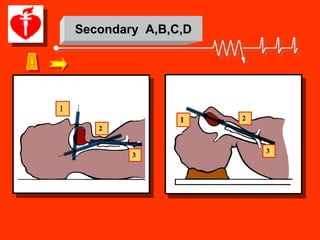
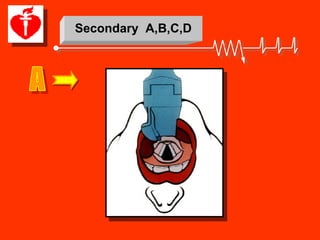
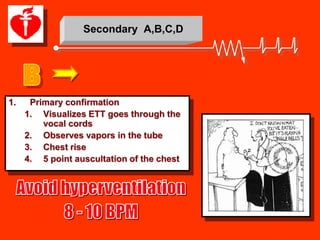
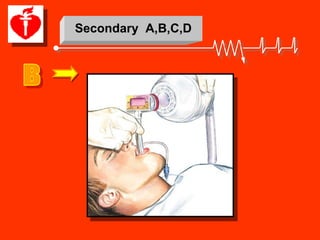
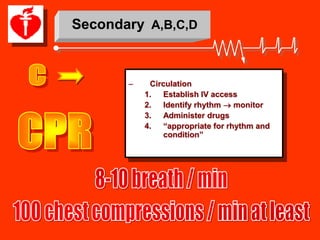
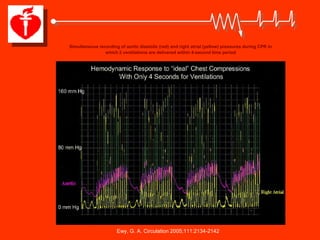
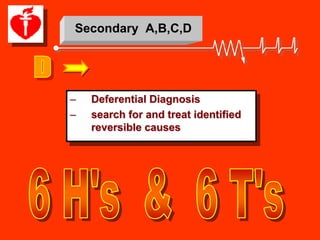
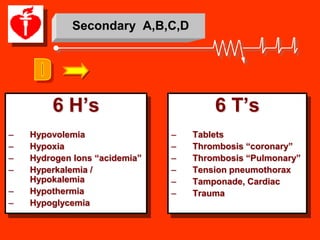
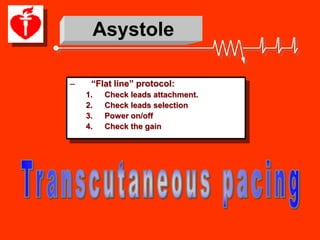
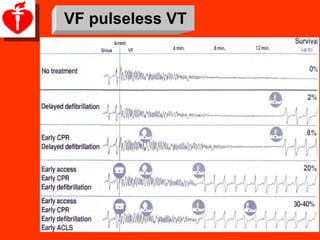
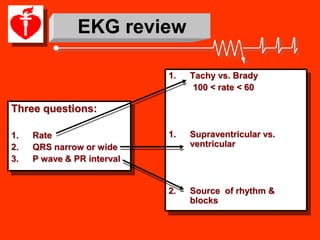
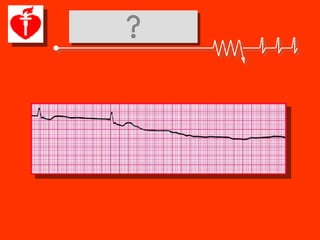
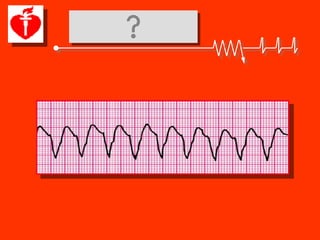
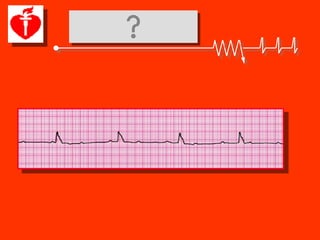
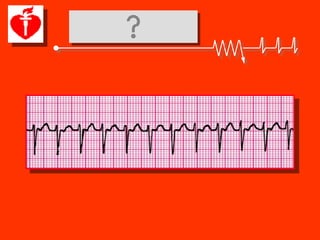
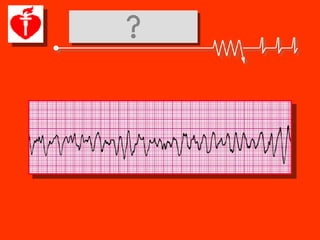
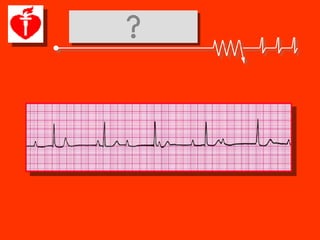
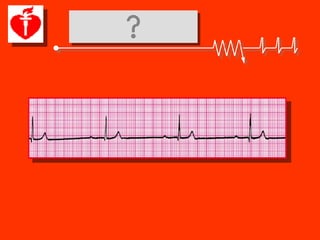
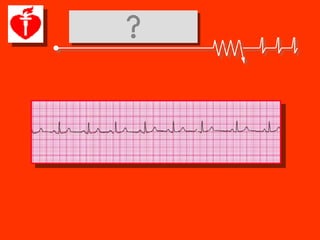
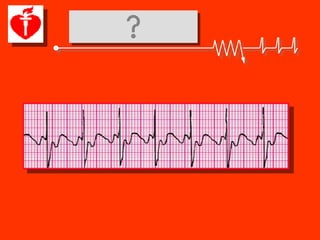
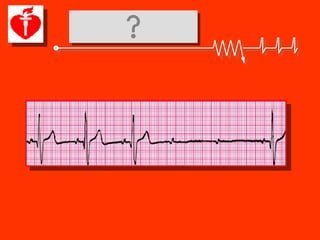
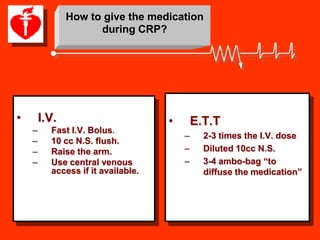
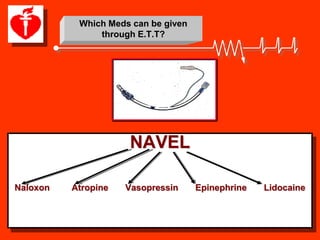
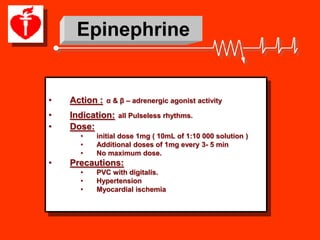
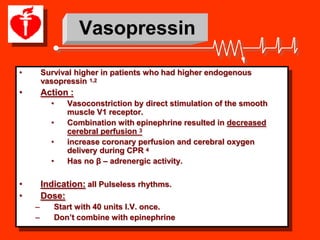
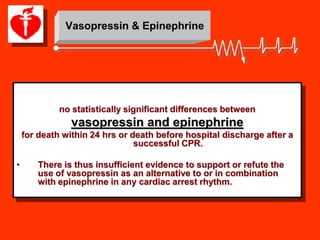
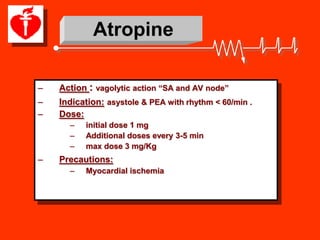
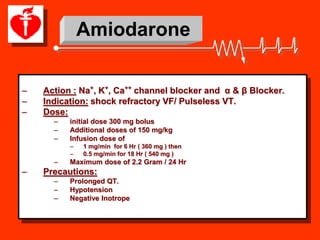
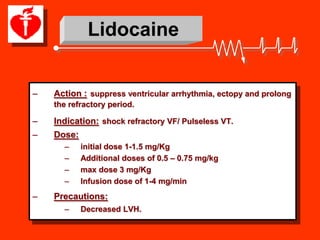
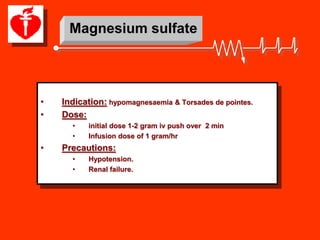
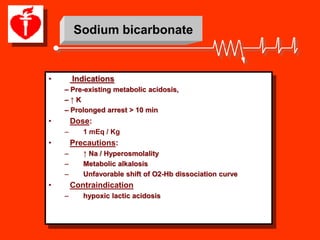
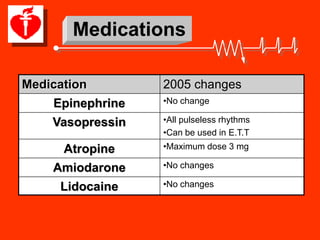
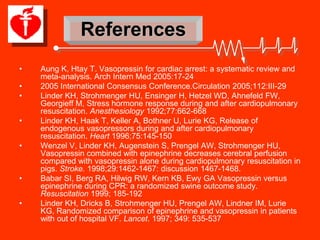
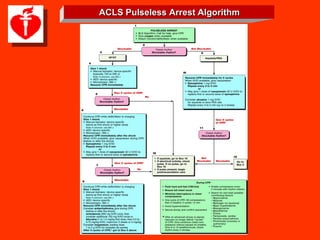
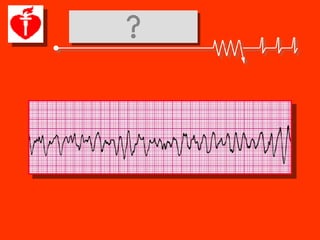
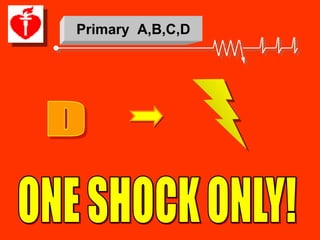
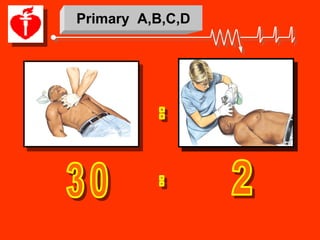
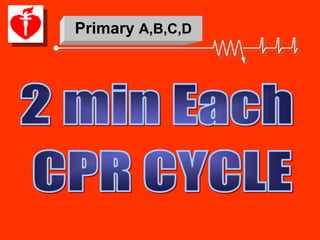
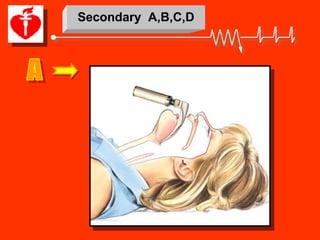
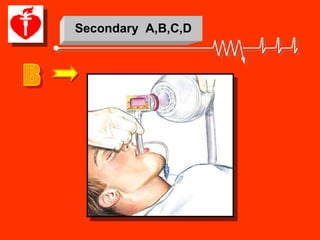
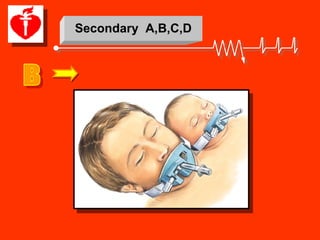
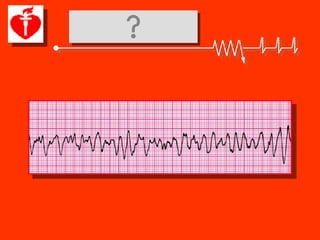
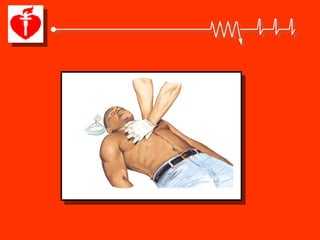
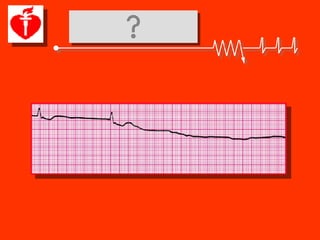
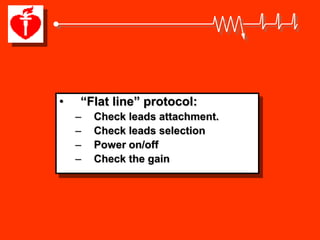
The document extensively reviews advancements in Advanced Cardiac Life Support (ACLS) focusing on critical EKG rhythms and the associated drug protocols for cardiac arrest management, particularly emphasizing the administration of medications like epinephrine, vasopressin, atropine, and amiodarone. It outlines the algorithms for pulseless arrests and the importance of identifying reversible causes of cardiopulmonary events. Additionally, it evaluates the implications of recent guidelines and research findings in the context of CPR and drug effectiveness.