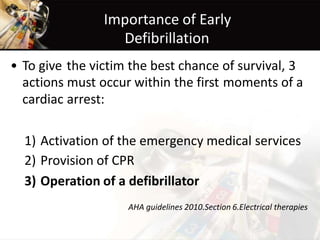
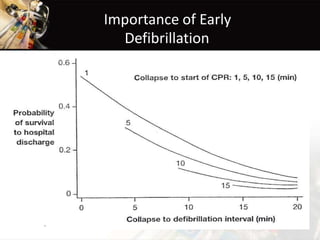
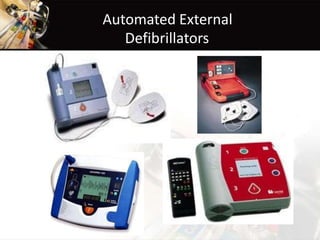
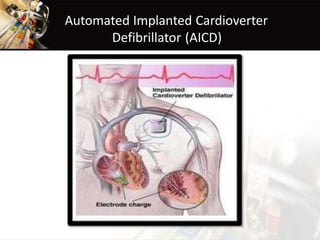
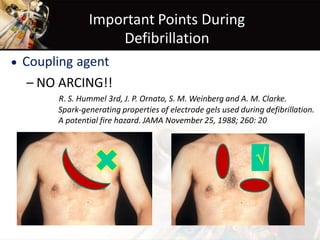
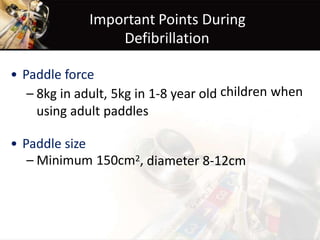
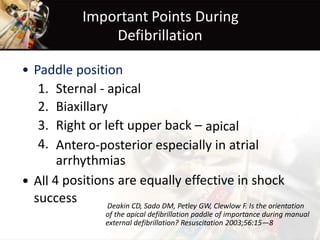
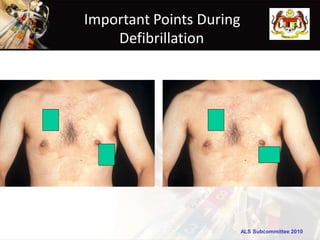
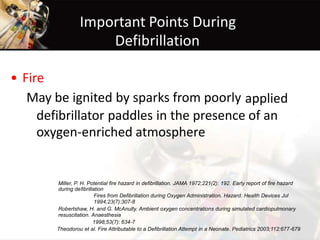
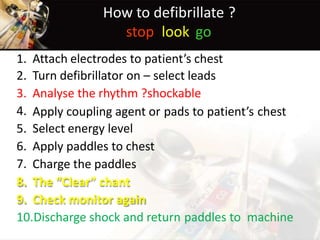
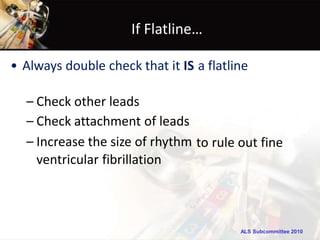
Defibrillation is a process that delivers an electric shock to stop an irregular heartbeat and restore normal rhythm. Early defibrillation within the first few minutes of cardiac arrest is crucial for survival. Pioneers like Claude Beck developed the defibrillator and helped revive heart attack victims. Proper defibrillator use requires correct pad placement and force, as well as ensuring safety from fires and electrical hazards. The delivery of the shock must be coordinated to avoid potential dangers and maximize effectiveness.