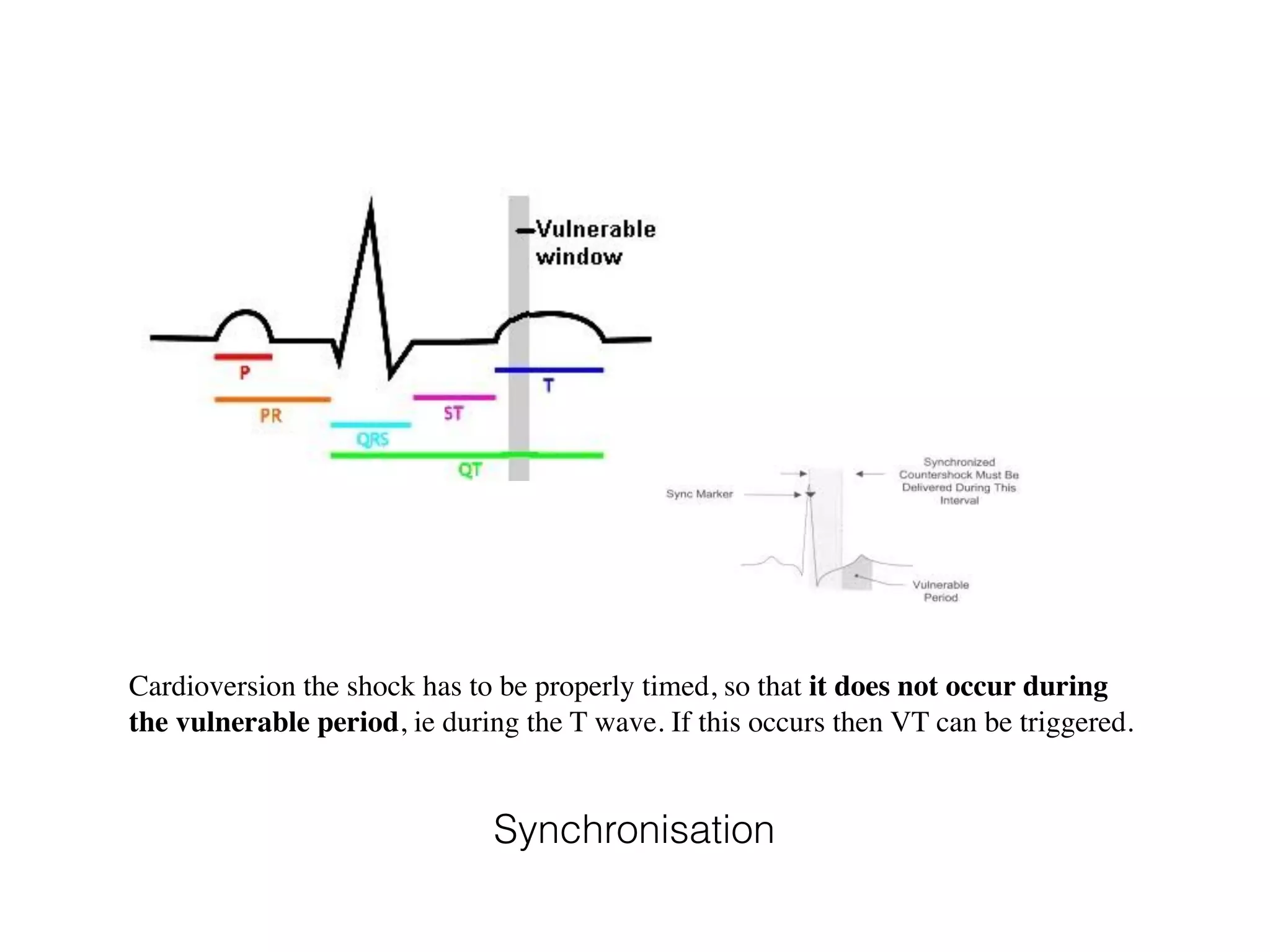
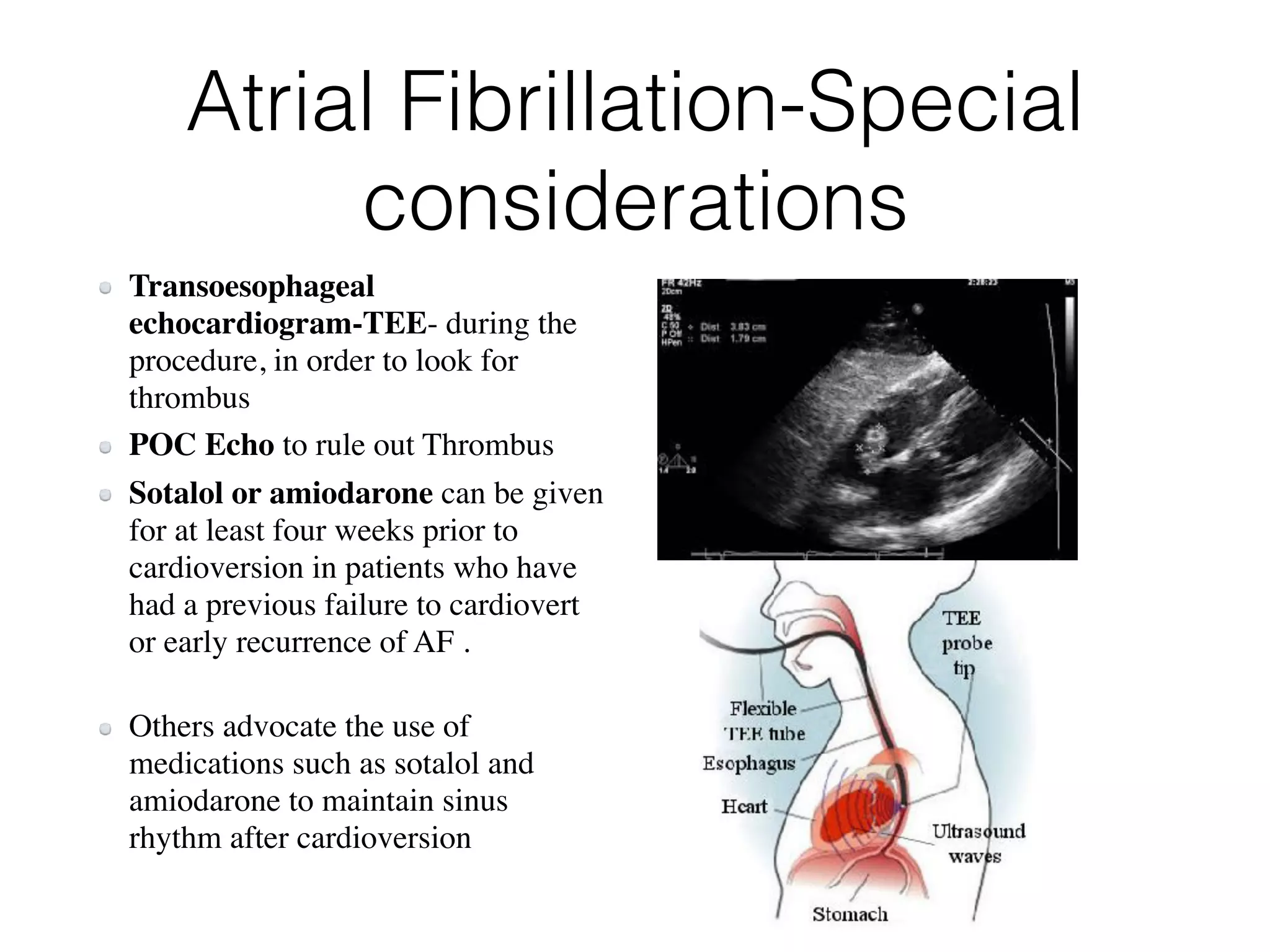
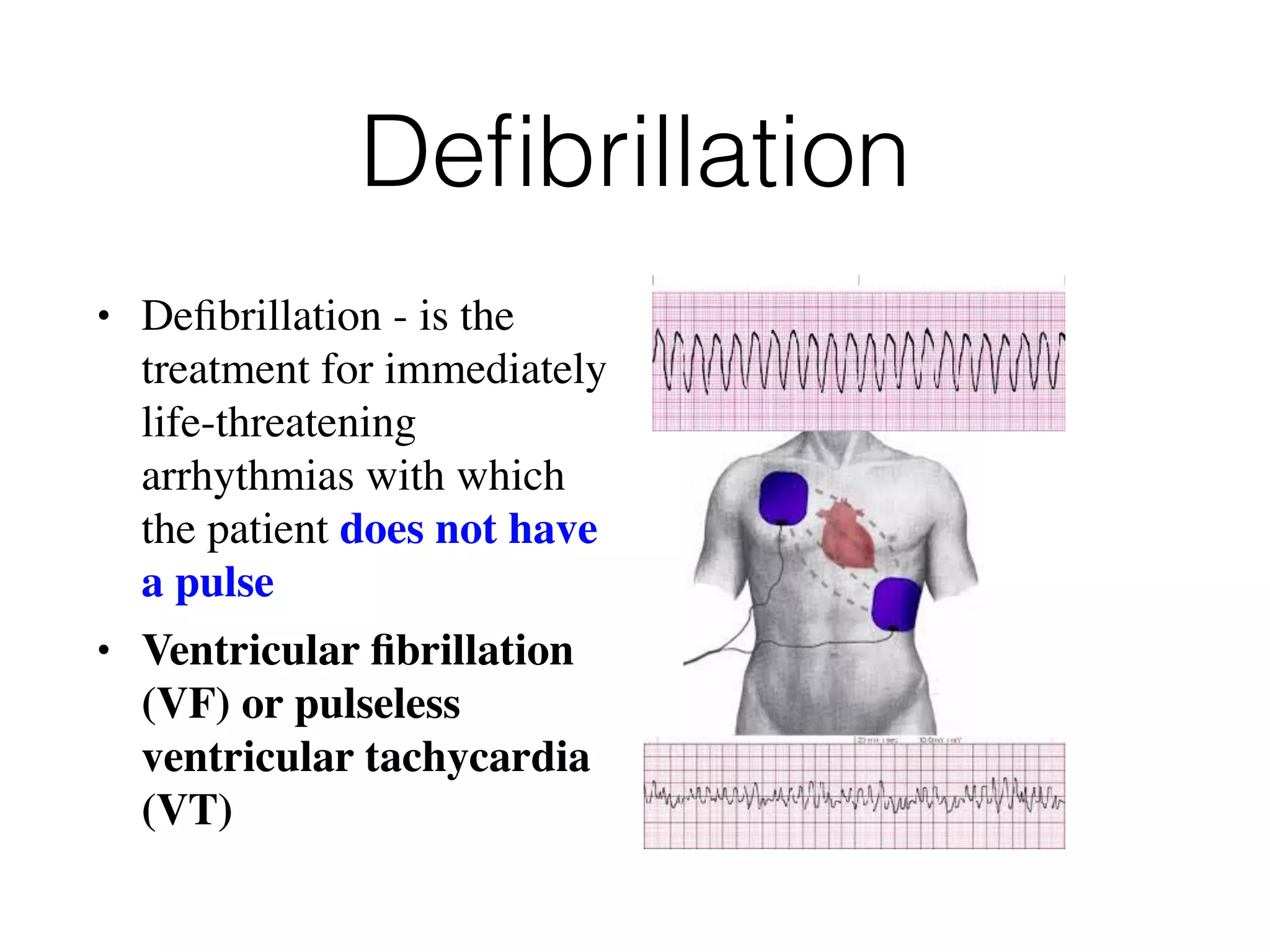
This document discusses defibrillation and cardioversion. It defines defibrillation as treatment for life-threatening arrhythmias without a pulse using electrical shock, while cardioversion aims to convert arrhythmias to normal rhythm with or without a pulse. Both use electrical energy to allow normal sinus rhythm. Defibrillation is for immediate use in ventricular fibrillation or pulseless ventricular tachycardia, while cardioversion may be used for unstable or failed chemical cardioversion of atrial fibrillation, atrial flutter, ventricular tachycardia with a pulse. The document reviews the history of defibrillation and types of defibrillators, and provides guidance on defibrillation and cardioversion procedures and considerations.








![Type of Defibrillators
• Automated External Defibrillators [AED]
• Semi- Automated AEDs
• Standard defibrillators with Monitor
• Trans-venous or Implanted defibrillators](https://image.slidesharecdn.com/defibandcardiovert-170615083645/75/Defibrillation-and-cardioversion-11-2048.jpg)